Cutaneous epidermal cyst



Clinical History
A 4-month history of a slowly enlarging subcutaneous mass in the left thigh. Clinical examination revealed a soft, well-defined, smooth mass subcutaneously in the anterior surface of the left thigh.
Imaging Findings
The patient presented with a 4-month history of a slowly enlarging subcutaneous mass in his left thigh. Clinical examination revealed a soft, well-defined, smooth mass subcutaneously in the anterior surface of the left thigh. The overlying skin was slightly protuberant, but apparently normal. Laboratory tests were normal.
MRI through the distal femur demonstrated a well-delineated ovoid mass within the subcutaneous fat anterior to the muscles and superficial fascia measuring approximately 4.5cm in diameter.
On axial T1-weighted spin echo MR images (TR/TE: 640/17) the lesion showed low to intermediate signal intensity with peripheral ill-defined amorphous areas of hyperintensity. Fast spin echo axial T2-weighted images using a fat suppression technique (TR/TE: 3000/25) demonstrated a mass with high signal intensity and peripheral low signal intensity areas. There was a partial hypointense rim on both T1- and T2-weighted images. After the administration of paramagnetic agent the mass remained unenhanced.
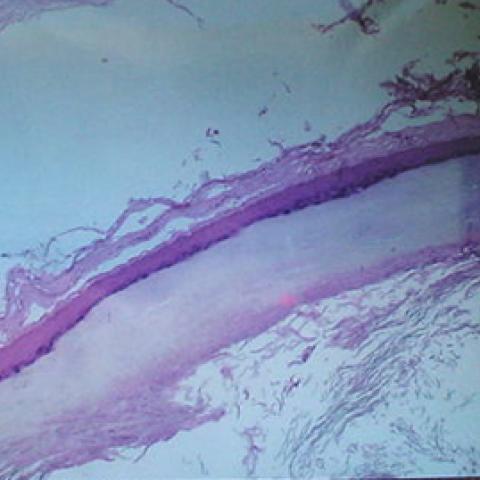
At operation the mass was found to have a thin wall and was mobilised quite easily from surrounding tissues. Histological examination showed an epidermoid cyst with layers having squamous and granular cells containing proteinaceous material, keratin and lipids.
Discussion
Epidermoids are inclusion cysts that arise from ectodermal cell rests and consist of stratified squamous epithelial linings surrounding desquamated keratin. As the contents slowly accumulate, the lesion often reaches considerable size. Epidermal cysts are usually diagnosed during the third or fourth decades of life and show a slight male predilection.
Although these cysts can occur anywhere in the body, they are most common in the head and neck area, orbit, nasal and oral cavity, and calvarial diploic space as well as intracranially in the middle and posterior fossa and intraspinally to the lumbosacral area [1-2].
Congenital epidermoid cysts are related to inclusion of ectoderm, with or without dermal elements, at the time of closure of the neural tube, between the 3rd and 4th weeks of foetal life. This accounts for the midline location of most cysts, and their possible association with defects of the overlying bone and skin. They can also occur as a result of traumatic implantation that forces skin tissue to be trapped in the subcutaneous tissue (e.g. iatrogenic or puncture wounds). It is estimated that 45% of intraspinal epidermoid tumours are iatrogenic. They are seen after single or multiple lumbar punctures and consequent deposition of skin fragments.
Cutaneous epidermoid cysts are very common; they are usually small, intradermal or subcutaneous lesions, so radiological examination is rarely performed. Cutaneous epidermoid cysts are one of the clinical features of Gardner's syndrome [3]. Rarely, epidermoid cysts reach a size larger than 5cm in diameter [2]. Such cases may be confused with soft tissue neoplasm. Malignant transformation of cutaneous epidermal cysts is rare. However, cases have been reported in the literature of neoplastic transformation of the epithelium, emphasising the importance of routine histology in excision of these lesions [4].
Magnetic resonance imaging is the study of choice for diagnosis of epidermal cysts. They have been reported in the literature to show low signal intensity on T1-weighted images and high signal intensity on T2-weighted images. They may be homogeneous or heterogeneous. Contrast enhancement has been occasionally described as a thin rim. Atypical features include high signal on T1 and low signal on T2-weighted images probably caused by inner dense keratin debris and cholesteror crystals. Not uncommon epidermoids have peripheral hypointense rim corresponding hystologically to a fibrous wall.
Recent papers focus on the value of diffusion-weighted imaging (DWI) in differentiating epidermoid from other cystic lesions. The apparent diffusion coefficient (ADC) of epidermoid cysts is usually significantly lower than that of CSF, consistent with restricted diffusion, indicating a solid lesion [5].
The differential diagnosis of cutaneous epidermoid on MRI includes ganglion cyst and soft tissue tumours with a cystic appearance such as myxoid liposarcoma. Ganglion cysts are homogeneous lesions, usually multicystic and in contiguity with tendon sheaths and joint capsules. The fact that soft tissue neoplasms usually enhance after the administration of paramagnetic agent strongly suggested the diagnosis in this case.
The treatment of choice for epidermal cysts is surgical excision for large or symptomatic masses.
Differential Diagnosis List
Final Diagnosis
Cutaneous epidermal cyst
Liscense
Figures
MRI through the distal left femur




Histological examination of epidermal cyst
Medical Imaging Analysis Report
I. Imaging Findings
1. Location and Morphology: Imaging reveals a round or oval lesion located in the subcutaneous tissue on the anterior aspect of the left thigh. The lesion has a well-defined boundary, exhibits overall soft tissue density/signal, and is clearly demarcated from the surrounding muscles and soft tissue.
2. Signal and Density Characteristics: On T1-weighted images, the lesion primarily appears as low or isointense, while on T2-weighted images, it demonstrates high signal intensity, suggesting a high water or protein content. Some slices show signal heterogeneity, potentially related to keratinous material or cholesterol crystals.
3. Enhancement Pattern: No obvious enhancement is observed on contrast-enhanced scans; the lesion may show mild or thin peripheral enhancement. Overall, the features are consistent with a cystic lesion containing keratin or dermoid components.
4. Involvement of Surrounding Tissues: The lesion is located subcutaneously, with no evident damage to muscles or bones. The surrounding soft tissue structures remain largely intact, with only mild local compression or deformation.
II. Possible Diagnoses
Based on the patient’s clinical presentation (a slowly growing, painless subcutaneous mass on the anterior aspect of the left thigh) and imaging findings, the following are possible diagnoses:
- 1. Epidermoid Cyst: Commonly found in subcutaneous tissue and soft tissue, typically slow-growing. On MRI, it often shows low signal on T1 and high signal on T2. Enhancement is usually absent or limited to thin rims, consistent with this case.
- 2. Ganglion Cyst: Commonly appears near joints or tendon sheaths, showing high signal on T2-weighted images. However, it typically communicates with a tendon or joint capsule, and a solitary cyst in the anterior thigh subcutis is relatively less common.
- 3. Soft Tissue Tumor (e.g., Myxoid Liposarcoma): May present as high T2 signal on MRI, but larger lesions often show irregular septations and marked enhancement; clinically, they are more aggressive.
III. Final Diagnosis
Taking into account:
- Patient age (35-year-old male), history (slow growth over 4 months), and clinical palpation (soft, well-circumscribed, and mobile),
- MRI characteristics (low/iso signal on T1, high signal on T2, well-defined margin, minimal enhancement),
- Likely presence of keratinous debris or squamous epithelial lining on histopathology,
The findings most closely align with an epidermoid cyst. Surgical intervention and pathological examination could provide a definitive diagnosis while also ruling out any rare malignant changes.
IV. Treatment Plan and Rehabilitation
1. Treatment Strategy:
For an epidermoid cyst that is large, symptomatic, or raises cosmetic concerns, complete surgical excision is recommended. Small and asymptomatic cysts may be observed; however, considering possible recurrence, infection, or the extremely rare malignant transformation, surgical removal and pathological evaluation are generally advised.
2. Rehabilitation and Exercise Prescription:
For patients encountering local discomfort prior to or after surgery, an individualized and gradual exercise plan following the FITT-VP principle is recommended:
- Type: Low-intensity aerobic exercises (e.g., walking, stationary cycling) and light resistance training.
- Frequency: 3–5 sessions per week.
- Intensity: Keep heart rate at 50%–60% of maximum heart rate for healthy adults as a starting point; choose light loads for resistance training.
- Time: 20–30 minutes per session, increasing gradually based on tolerance.
- Progression: With wound healing and improved fitness, aerobic sessions can be extended to 30–45 minutes, and resistance load can progress from light to moderate, avoiding stress on the surgical area.
- Volume & Pattern (Precautions): If the surgical site is on the anterior thigh, avoid excessive flexion or extension under load in the early postoperative period. Resume major muscle group training only after proper healing.
During early postoperative wound healing, pay close attention to infection control and avoid forceful stretching. If redness, discharge, or worsening pain occur in the wound area, seek medical attention promptly.
Disclaimer: This report is based solely on the provided images and limited clinical information. It is for reference only and does not substitute for an in-person consultation or professional medical advice. If you have any questions, please consult a specialist and undergo further examination and evaluation.
Human Doctor Final Diagnosis
Cutaneous epidermal cyst