


The patient presented with complaints of low back pain on the left side, which had become progressively worse.
The patient presented with complaints of low back pain on the left side, which worsened progressively. On examination she was found to have reduced lumbar mobility, a reduction in straight leg raising on the left to 70%, normal reflexes and normal motricity and sensation.
CT of the spine revealed degenerative changes with lower disc bulging and facet joint arthropathy (Fig 1).
MRI showed an extradural left-sided posterolateral cystic lesion at the L3-L4 level that was isointense on T1-weighted images and markedly hyperintense on T2-weighted images. It was well defined and closely related to the facet joint. Hypertrophy of the adjacent facet joint with hyperintense intra-articular fluid effusion compared to the right side was seen. A linear high signal communication was seen between the cyst and the intraarticular fluid effusion. After the administration of paramagnetic agent, enhancement of the cyst wall was seen (Fig. 2).
A preoperative diagnosis was made of a synovial cyst arising from the facet joint, and this was confirmed by a pathological examination obtained at surgery. The patient made an excellent recovery with complete pain relief.
Synovial cysts (SCs) arising from the facet joint of the lumbar spine is rare and was first described by Kao et al. in 1968. Over the last few years SCs have been increasingly reported, probably because of the availability of CT and MRI. SCs represent an enlargement of the articular synovial capsule in the spinal canal. True SCs communicate with the facet joint and are composed of a fibrous capsule lined by synovium. The aetiology of SCs is thought to be linked with degenerative change (osteoarthritis and rheumatoid arthritis) and excessive mobility (spondylolisthesis), which would account for their most frequent occurrence in the lower lumbar spine. The accepted mechanism for the pathogenesis of these lesions is excessive joint mobility with herniation of the synovium through a defective joint capsule.
In a study of Tillich et al. 72% of SCs were located at the L4-L5 level, 17% at the L5-S1 level and 11% at the L3-L4 level.
The symptomatology depends on the size and location of the cyst. The usual symptom is intermittent lumbar pain, with or without radiculopathy. Neurological deficits are infrequent. Presentation with cauda equina syndrome or with sudden pain exacerbation may be caused by intracystic bleeding with an abrupt increase in the size of the cyst.
On CT, synovial cysts may be seen as hypodense, well-delineated cystic masses adjacent to the facet joint. As the lesions have equal density with cerebrospinal fluid in many cases it is difficult to see them, as in this case where, even retrospectively, it was impossible to detect the cystic mass.
On MRI synovial cysts are smooth, extradural, well-circumscribed cystic masses arising adjacent to the facet joint. Synovial cysts without haemorrhage appear isointense, or slightly hyperintense, relative to the cerebrospinal fluid on T1-weighted images and hyperintense on T2-weighted images. There are different theories regarding the slight hyperintensity relative to CSF. Based on laboratory findings, it was postulated that the fluid within the cyst might have higher protein content. However, the higher relative signal intensity in the cyst may be due to the lack of motion-induced signal loss in the encapsulated cystic fluid compared with the circulating CSF in the subarachnoid space. Another possible explanation is that small amounts of paramagnetic breakdown products may be present in the cyst fluid. In some cases, haemorrhage into the cyst occurs followed by peripheral and internal calcification within the lesion. A low signal intensity may be seen at the rim of a haemorrhagic cyst on T2-weighted images due to the presence of a fibrous capsule with haemosiderin deposits. MR imaging rarely reveals demonstrable communication with the facet joint.
Associated imaging findings include degenerative disc disease, advanced osteoarthritic changes with hypertrophy of the facet joints and thickening of the ligamentum flavum at the level of the SC. Fatty replacement as well as osteosclerosis of the bone marrow in the posterior elements adjacent to the SC is also seen.
The MR imaging features and associated findings of synovial cysts are helpful in differentiating them from other lesions. The differential diagnosis of SCs in the lumbar spine includes schwannoma, migrated herniated disc fragment, extradural arachnoid cyst and perineural cyst.
Treatment of synovial cyst usually consists of surgical resection, percutaneous injection, aspiration and immobilisation using a brace. Surgery is a safe and effective treatment for patients with a lumbar SC and is the treatment of choice for such lesions. However, a few reports have described a dramatic decrease in the size of a SC and even complete disappearance during the operation, compared with its appearance on initial MR images. Otherwise surgical decompression is indicated in the presence of progressive pain and neurological deficit.
Lumbar facet joint synovial cyst




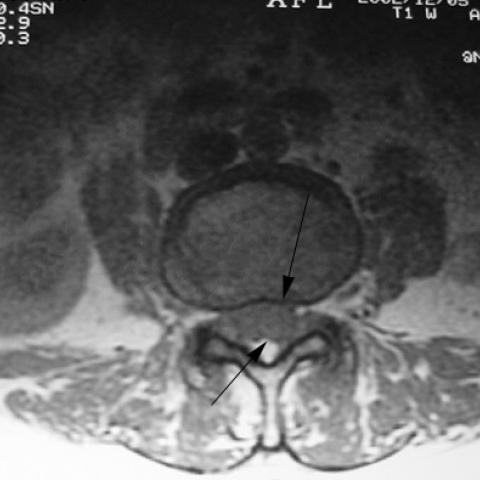



According to the patient’s CT and MRI images, a cystic lesion with relatively well-defined margins is visible in the lower lumbar spine (most commonly at the L4-L5 level). It is located posteriorly in the spinal canal and adjacent to the facet joint. On MRI sequences, the lesion typically shows iso- or slightly hyperintense signals on T1-weighted images and hyperintense signals on T2-weighted images, clearly contrasting with surrounding spinal canal structures. Some images suggest soft tissue thickening or degenerative changes adjacent to the facet joint (e.g., facet hypertrophy, ligamentum flavum thickening). Currently, there is no significant evidence of spinal canal stenosis causing acute spinal cord compression, but the relatively large size of the cystic lesion exerts a certain mass effect.
Some images do not clearly demonstrate a direct connection between the cyst wall and the joint capsule; however, the position of the cyst is highly consistent with a typical synovial cyst adjacent to the facet joint. Local degenerative changes (bony sclerosis, irregular joint surfaces) further support the correlation between degenerative changes and the formation of synovial cysts.
Based on imaging features and the patient’s symptoms of low back pain, the following diagnoses or differential diagnoses may be considered:
Taking into account the patient’s age (59), progressively worsening chronic low back pain, imaging findings showing a cystic lesion at the facet joint, and local facet joint degeneration, the most likely diagnosis is lumbar facet joint synovial cyst (Synovial Cyst).
Before or after surgery (if required), a staged rehabilitation program can be implemented according to pain level and range of motion. Below is a reference plan based on the FITT-VP (Frequency, Intensity, Time, Type, Volume, Progression) principle:
If the patient has comorbidities such as osteoporosis, hypertension, or poor cardiopulmonary function, the exercise prescription should be modified under the guidance of a physician or rehabilitation therapist to avoid the risks associated with falls or excessive strain.
This report provides a reference opinion based on the current images and patient history and does not replace in-person consultation or professional medical advice. If you have any questions or changes in your condition, please seek prompt medical attention and consider further examinations or consult with qualified healthcare professionals.
Lumbar facet joint synovial cyst