Common peroneal nerve compression by the extraosseous component of an intraosseous ganglion cyst of the fibular head.



Clinical History
Paresis of left peroneal nerve since four months, with a lytic lesion at the head of the fibula.
Imaging Findings
A middle-aged woman presented to our hospital because of pain at the lateral aspect of the knee joint, steadily worsening during the last four months. The neurological examination showed paresis of the left common peroneal nerve.
Radiographs of the left knee revealed a lytic lesion at the head of the fibula surrounded by a sclerotic rim (fig.1). There was some expansion of the medial aspect of fibular head but no cortical breech was seen.
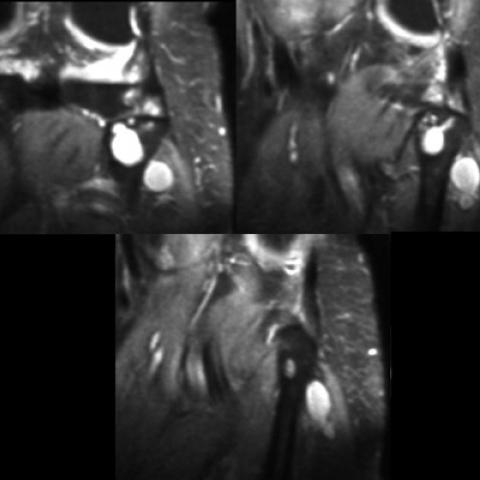
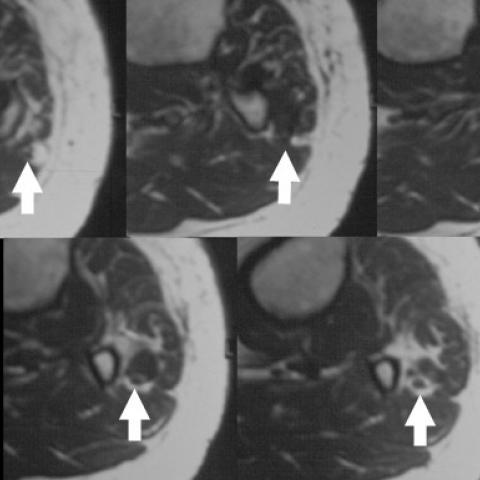
A subsequent MRI showed the lesion to be cystic (fig. 2, 3). A cortical breech through the frontal aspect of the fibular head was disclosed (fig.4), through which, the lesion extended out of the bone laterally compressing the common peroneal nerve between the extraosseous component of the lesion and the neighboring peroneous longus muscle (fig.4).
A surgical excision was decided in order to prevent further neurological damage to the peroneal nerve.
Histologically the lesion was found to represent a ganglion cyst. The patient recovered well and she was pain free and without neurological compromise during the follow-up examination three months after surgery.
Discussion
Ganglion cysts may arise de novo within a bone as intraosseous ganglion cysts [1,2]. Histologically they are not true cysts because they do not possess epithelial lining. The intraosseous ganglion generally does not communicate with the neighboring joint [1]. The differential diagnosis of an intraosseous cystic lesion at the vicinity of a joint in a long bone, besides an intraosseous ganglion, includes degenerative subchondral bone cyst, chondroblastoma, aneurysmal bone cyst, giant cell tumour of bone, and pigmented villonodular synovitis [1,2,3]. The degenerative subchondral bone cyst is a benign lesion which radiographically appears as a lucent well defined lesion surrounded by a sclerotic rim [1]. No cortical expansion is observed. Degenerative changes of the neighboring joint are shown. It is found in the elderly or post traumatic patients.
Intraosseous ganglion is similar radiographically to the degenerative subchondral bone cyst, but degenerative changes of the neighboring joint are not found, and it has a predilection for the middle-aged persons.
Chondroblastoma, aneurysmal bone cyst, and giant cell tumour of bone are mainly found in adolescents and young adults and do not show continuity with the neighboring joint [1].
Pigmented villonodular synovitis appears at both sides of a joint [1,2].
In our case the lesion was lucent, it had a sclerotic border, small expansion of the fibular head was noted, and there was no involvement of the proximal tibiofibular joint.
Around the knee joint, cystic lesions of the soft tissues include intraneural ganglion, synovial, and ganglion cysts. There are differences in pathology between these entities, and different theories explaining their origin and formation have been proposed. Intraneural ganglion cysts arise within the perineurium of a peripheral nerve [4]. Synovial cysts originate from the synovium and usually communicate with the parent joint. Most authors report that ganglion cysts result from myxoid degeneration of connective tissues because they are usually located in areas of physical stress [2]. Some authors report that these cysts are formed from displacement of synovial tissue during embryogenesis, and others suggest that they arise from the articular capsule [5].
From a therapeutic point of view it is important to know whether these lesions abut the perineurium or communicate with the parent joint, because these findings change the therapeutic approach [2,5].
MR imaging is very helpful preoperatively because it can disclose the anatomic relationships between the lesion and the neighboring structures [5]. If ganglion cysts are located close to nerves, they may provoke symptoms because of compression, resulting in pain and sometimes in nerve compromise [1,4]. Intraosseous ganglia, on the other hand, do not cause symptoms, unless they expand the cortex and subsequently compress neighboring organs [4]. It is rare for an intraosseous ganglion to breech the cortex and extend beyond bone to compress the surrounding soft tissues [3,4]. In our case, MRI revealed an intraosseous ganglion with an extraosseous component which compressed the common peroneal nerve and caused the patient's symptoms.
Differential Diagnosis List
Final Diagnosis
Common peroneal nerve entrapement
Liscense
Figures
AP radiography of the left knee

Coronal T1W/SE

Coronal T2W/TSE
Axial T1W/SE
Medical Imaging Analysis Report
I. Imaging Findings
1. From the anteroposterior and lateral X-ray views of the knee, a radiolucent lesion is observed in the region of the left fibular head. The lesion has a relatively well-defined margin with surrounding sclerosis; there is a slight expansion of the fibular head, with no obvious cortical destruction or collapse.
2. MRI (coronal and axial views) shows a cystic signal within the fibular head, appearing low to intermediate on T1 and relatively high on T2-weighted images. The lesion extends outward from the bone, forming a cystic structure adjacent to and compressing the common peroneal nerve. There is no obvious connection with the adjacent joint.
3. No significant fracture lines or large-scale inflammatory or erosive changes in the soft tissues are noted. The surrounding soft tissues appear relatively normal, except for clear signs of compression along the course of the common peroneal nerve.
II. Differential Diagnosis
- Intraosseous Ganglion of the Fibular Head: These lesions typically present as radiolucent areas with well-defined margins and a sclerotic rim, often seen in middle-aged adults, possibly with mild expansion. They usually do not connect with the joint. If the cyst extends beyond the bone, it may compress surrounding structures.
- Degenerative Subchondral Bone Cyst: Commonly seen in patients with degenerative joint disease or a history of trauma, often accompanied by signs of adjacent joint degeneration (e.g., joint space narrowing, osteophyte formation). This is more frequent in older patients, and imaging typically shows adjacent degenerative changes.
- Other Bone Lesions (such as enchondroma, giant cell tumor, aneurysmal bone cyst, etc.): These lesions frequently occur in adolescents or young adults, and imaging may show more pronounced bone destruction, septations, or irregular boundaries. Given the patient’s age and the imaging features, these are relatively less likely.
III. Final Diagnosis
Considering the patient’s age (43 years), clinical presentation (mild common peroneal nerve palsy in the left leg for four months), and imaging findings (a radiolucent cystic lesion with a sclerotic rim in the fibular head, slight expansion compressing the common peroneal nerve), the most likely diagnosis is:
Intraosseous Ganglion of the Fibular Head with Extension Outside the Bone, Compressing the Common Peroneal Nerve.
Surgical exploration and pathological examination may be required for definitive diagnosis and to rule out any other rare entities.
IV. Treatment Plan and Rehabilitation
1. Treatment Strategy
- If symptoms are significant, if there is severe nerve compression, or if progressive neural deficits are present, surgical intervention is recommended. This may include lesion excision or surgical decompression along with exploration of the common peroneal nerve to ensure adequate decompression.
- If symptoms are mild and non-progressive, conservative management can be considered, including regular follow-up to monitor lesion size and nerve function. However, vigilant observation for any worsening of neurological symptoms is essential.
- If there is an intra-articular communication (rare) or a synovial cyst component found during surgery, related joint pathology should be considered, with arthroscopic evaluation as appropriate.
2. Rehabilitation / Exercise Prescription Recommendations
The goals of the rehabilitation plan include reducing local inflammation, protecting the function of the common peroneal nerve, and restoring muscle strength and range of motion of the affected limb. The program can be carried out in stages as follows:
- Early Postoperative or Initial Conservative Phase (Week 1–2):
- Focus on pain relief and reduction of soft tissue swelling. Low-intensity physical modalities (e.g., intermittent cold packs, ultrasound therapy) and nerve mobilization techniques may be applied.
- Avoid prolonged weight-bearing on the affected limb if necessary. Use crutches or a brace to protect the common peroneal nerve area.
- Intermediate Rehabilitation Phase (Week 2–6):
- Gradually introduce lower-limb strengthening exercises, such as active ankle dorsiflexion, plantar flexion, and overall coordinated exercises. Emphasis should be placed on activating the anterior tibialis and peroneal muscle groups.
- Engage in low-intensity stability training, starting with double-leg balance exercises and progressing to single-leg balance training to improve coordination and neuromuscular control.
- Apply the FITT-VP principle: 3–4 sessions per week, each lasting 20–30 minutes, at low to moderate intensity. Adjust based on pain threshold and fatigue levels.
- Advanced Strengthening Phase (Week 6 onward):
- Once pain and neural symptoms have subsided, increase the intensity of resistance exercises. This may include using resistance bands or light-to-moderate weights for ankle dorsiflexion exercises.
- Commence closed-chain functional training (e.g., partial squats, lunges) as tolerated, while closely monitoring nerve symptoms and joint stability.
- Apply the FITT-VP principle: 3–5 sessions per week, each lasting 30–45 minutes, at moderate intensity. Gradually increase load based on individual progress.
- Reassessment and Progression:
- Regularly evaluate nerve function (muscle strength testing, gait analysis) to determine if the exercise program needs to be modified.
- If the patient experiences increased pain or deterioration of neural function, prompt medical consultation is advised and the training plan should be adjusted accordingly.
Note: If the patient has other comorbidities (e.g., osteoporosis, poor cardiopulmonary function), adjustments to exercise intensity and frequency should be made, and professional medical supervision is recommended to ensure safety.
Disclaimer: This report is based solely on the provided imaging data and clinical information, serving as a reference rather than a substitute for in-person evaluations or the opinions of qualified medical professionals. In case of any questions or changes in condition, please promptly consult orthopedic, radiology, or other relevant specialists.
Human Doctor Final Diagnosis
Common peroneal nerve entrapement