A case of bilateral severe congenital coxa vara diagnosed in late stage


Clinical History
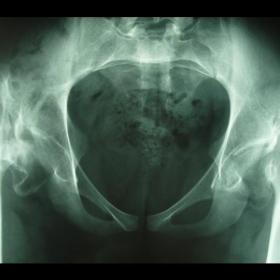
Radiographic and computed tomographic findings of a 21-year-old male patient with a painless waddling gait, were presented.
Imaging Findings
A 21-year-old male patient presented with a waddling gait, without pain. He had begin to walk at the age of two and a half years, and he had had a walking disorder since then. He was diagnosed as suffering from a sequel of developmental dysplasia of the hip (DDH) in his early childhood. The anteroposterior pelvic radiographs which were taken, showed that the proximal part of both femurs were displaced superiorly, but the development of both acetabuli was normal and the femoral heads were confined well within the acetabulum (Fig. 1). Axial computed tomographic (CT) images revealed normal femoral head and acetabular development in both hips, while femoral heads were within the acetabulum but the femoral shafts were displaced superoposterolaterally. Both femoral heads were partially osteoporotic and their contours were found osteosclerotic on the lateral fragmented site (Fig. 2). Three-dimensional (3D) reconstructed CT images clearly identified that the femoral shafts and femoral heads were completely separated from each other and there was no pseudoarticulation between the proximal femur and the iliac bone on both sides (Fig. 3).
Discussion
Coxa vara is a hip deformity caused by a decreased angle between the femoral neck and shaft to less than 120º as measured on an anteroposterior radiograph. The normal femoral neck-shaft angle in children changes with age. The femoral neck is valgus in the infant because of the relatively increased growth of the medial portion of the physis during the perinatal period, and the angle value is approximately 150º at the time of birth. During childhood, there is a greater amount of growth in the lateral portion of the femoral physis and the femoral neck-shaft angle, decreasing gradually to a value of 120º in the adults. Congenital coxa vara (CCV) is caused by an abnormality in the development of the proximal femoral physis, and defective ossification of the adjacent metaphysis that is influenced by weight-bearing which are responsible for the progressive decrease of the femoral neck-shaft angle. It is often bilateral and noticed when the child begins to walk. During early childhood, it presents with progressive, pain free gait abnormalities, and commonly follows a clinical course progressively with growth. The patients with bilateral CCV commonly present with waddling gait abnormalities. Histological studies have shown abnormalities in enchondral bone formation, which resemble those seen in metaphyseal chondrodysplasia, but are limited to the proximal femoral physis. On physical examination, hip abduction and rotation is found to be limited and there is a marked rising of the greater trochanter. Radiographically, the angle between the femoral shaft and the neck is found to be less than 120º. A characteristic finding of an inverted Y-shaped lucency is seen in the inferior part of the neck with the small triangular corner fractures. CT scans and 3-D reconstructed images may provide useful information for differential diagnosis and pre-operative surgical planning. MR imaging reveals that a widening of the physis has been demonstrated with the expansion of the cartilage. In untreated cases, progressive deformities also occur in the femoral head and the acetabulum, leading to the loss of hip function with the development of premature degenerative changes. We did not detect any remarkable degenerative changes in the present case. We thought that it may be related to the protection of the femoral head from weight-bearing, because of the complete separation of the femoral head and shaft.
Differential Diagnosis List
Final Diagnosis
Congenital coxa vara.
Liscense
Figures
Direct radiography

CT

3D CT

Medical Imaging Analysis Report
I. Imaging Findings
From the provided pelvic anteroposterior X-ray, CT axial slices, and 3D reconstruction images, the following can be observed:
- The angle between the femoral neck and femoral shaft on both sides is significantly reduced, estimated to be below 120°, suggesting a pronounced inward inclination of the femoral neck axis (i.e., Coxa Vara).
- There are developmental abnormalities in the bilateral hip joints, with shortened femoral necks. No distinct signs of acetabular overgrowth or bone destruction are observed.
- No obvious signs of joint surface degeneration or osteophyte formation; no evident joint space narrowing is noted.
- No significant soft tissue swelling or pathological density shadow is observed. The surrounding soft tissue appears essentially normal.
- No other obvious abnormalities are noted in the remaining pelvic area.
II. Potential Diagnoses
Considering the patient is 21 years old, presents with a painless waddling gait, and exhibits bilateral changes on imaging, possible diagnoses or differential diagnoses include:
- Congenital Coxa Vara: The most common indication is a bilateral decrease in the femoral neck-shaft angle. Patients often present with unsteady gait or limping in childhood. Imaging features typically show a femoral neck-shaft angle of less than 120° and other proximal femoral developmental abnormalities.
- Developmental Dysplasia of the Hip (DDH): This can also lead to abnormal gait patterns but usually involves acetabular dysplasia and an abnormal position of the femoral head. In this case, no obvious signs of a shallow acetabulum or other typical DDH changes are noted, making this diagnosis less likely.
- Other rare deformities due to epiphyseal or cartilaginous developmental anomalies: Conditions such as certain types of chondrodysplasia or metabolic bone diseases may cause abnormal hip morphology, though they often involve additional systemic or multiple skeletal manifestations.
III. Final Diagnosis
Based on the bilateral hip imaging findings, clinical presentation (painless waddling gait), and imaging features (a notably decreased femoral neck-shaft angle, approximately <120°), the most likely diagnosis is:
Congenital Bilateral Coxa Vara.
Currently, there are no evident signs of degenerative changes or joint destruction on imaging, indicating that the hip joints remain relatively stable, although there is a possibility of gradual progression over time.
IV. Treatment Plan and Rehabilitation Program
In light of the characteristics of congenital bilateral coxa vara, the treatment and rehabilitation strategies can be outlined as follows:
-
Conservative Management:
- If the patient’s daily activities are still manageable without significant pain or mobility restrictions, conservative monitoring may be considered initially.
- Regular follow-up (e.g., every 6–12 months) is recommended to monitor the femoral neck-shaft angle and joint space, keeping track of any onset of pain or worsening deformities.
-
Surgical Treatment:
- For patients with a pronounced deformity, severely limited gait function, or a progressive trend toward worsening deformity, an osteotomy (such as a proximal femoral corrective osteotomy) should be considered to restore a normal or near-normal femoral neck-shaft angle and improve weight-bearing alignment and range of motion.
- If acetabular dysplasia or secondary degenerative changes are detected, additional hip reconstruction procedures may be required accordingly.
-
Rehabilitation & Exercise Prescription:
- Early Intervention: During conservative or surgical treatment, guided functional training should be initiated as early as possible to prevent further loss of hip range of motion.
- FITT-VP Principle:
- Frequency: 3–5 rehabilitation sessions per week, gradually increasing based on the patient’s tolerance.
- Intensity: Begin with low-intensity joint mobility and small muscle group strengthening exercises. Increase gradually, adjusting to joint stability and pain levels.
- Time: Each session should last about 20–30 minutes. Initially, prolonged weight-bearing activities should be avoided, with an emphasis on proper form.
- Type: Focus primarily on low-impact exercises such as hip joint active movements performed in seated or supine positions, and resistance band exercises to maintain quadriceps and gluteal muscle strength. Progress to swimming, cycling, or other whole-body exercises.
- Progression: As joint range of motion and strength improve, gradually introduce weight-bearing training, such as supported standing balance exercises or simple squats with appropriate support.
- Volume and Pattern: Adhere to the principle of “small amounts multiple times, gradual transition.” Sessions can be divided into segments to allow adequate rest.
- Individualized Training: Given the special bilateral hip structure, avoid abrupt rotational or excessive twisting movements. Use supportive devices or walkers when necessary to reduce unnecessary external forces.
- Daily Living Guidance: Avoid prolonged weight-bearing activities (e.g., long periods of standing, heavy lifting). Pay attention to protective postures for the hips when sitting or sleeping.
Disclaimer: This report is a reference analysis based on the information currently provided and does not replace an in-person consultation with a professional physician or further examinations. If you have any questions or experience changes in your condition, please consult an orthopedic specialist for a more comprehensive diagnosis and treatment plan.
Human Doctor Final Diagnosis
Congenital coxa vara.