High frequency sonography and color-Doppler enhancement with a second generation contrast agent in the preoperative assessment of a melanoma



Clinical History
A man presented with a melanocytic nevus on the back. A sonographic study that was done showed he had a hypoechoic tumor. The tumor measured 3.55 mm in thickness. The color-Doppler showed intratumoral vascularization and after an injection of 2.5 ml of an intravenous contrast agent, it was found to be highly enhanced.
Imaging Findings
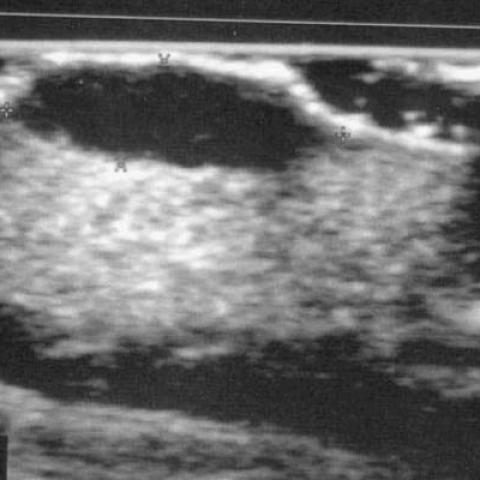
A 66-year-old man presented to his dermatologist with a melanocytic nevus that he had on his back from birth. During the past three months, before going to the dermatologist, it had started to grow without any symptomatology. On physical examination, no adenopathies were found. A sonographic study was done, before its extirpation, to measure the depth and the vascularization of the cutaneous lesion. The sonographic study was performed using an electronic transducer of 15 MHz with a sonoCT® and a Philips HDI 5000 equipment (Royal Philips Electronics Eindhoven, The Netherlands). The tumor was found to be hypoechoic with well-defined lateral and lower margins. The measurement between the lower margins of the hyperechoic line (Interphase gel-epidermis) to the deepest point of the distal margin was 3.55 mm in depth. (Fig. 1). The color-Doppler demonstrated intratumoral vascularization (Fig. 2). After the administration of 2.5 ml of an intravenous second-generation contrast (sonoVue ®), the lesion was seen to be highly enhanced (Fig. 3). The spectral analysis of the intratumoral vascularization showed a low resistive index: 0.53, which is characteristic of tumoral neovascularization (Fig. 4) being present. The tumor was surgically removed with a security margin of 2 cm. In the histological analysis, the tumor was found to be 3.05 mm in depth with an increase of its vascular-lymphatic structure using immunohistochemical staining with CD-31. Six months after the surgical removal, a left axillary mass with a maximum diameter of 4 cm was found. The mass was surgically removed by means of an incision resembling a wedge formation. In the histological analysis, the surgical piece was reported to be due to lymph recurrence. In the follow-up of the tumor, bilateral pulmonary metastasis was detected in the CT of the thorax enhanced with a contrast (Fig. 5). Three months later, a brain MRI demonstrated the presence of multiple supratentorial metastasis which affected both cerebral hemispheres with edema being associated. At present, the patient is being treated with interferon associated with holocranial radiotherapy to control the cerebral metastasis.
Discussion
Treatment for melanomas is based on the age and the general health of the patient, as well as, on the stage of the disease (Breslow index). Surgery is often sufficient to cure people with an early-stage melanoma. In the later stages of the disease, the surgery is generally followed with additional therapy (chemotherapy, radiation therapy or immunotherapy). In approximately 30% of the cases, the histological analysis shows a Breslow index, because of which, a new surgical removal is required. According to the Breslow index, the tumor depth determines the surgical margins, so for an index of 1 mm or less, the security margin would be 1 cm and 2 cm for those with an index between 1.01 mm and 2 mm and 3 cm for those with an index between 2.01 and 4 mm. Some studies have shown the accuracy of high frequency sonography with a mechanic transducer of 20 MHz in dermatology, especially in the melanoma previous evaluation before the surgery. A color-Doppler and sonographic first generation contrast agents can be used for the study of melanoma angiogenesis. We have used an electronic transducer of 15 MHz with sonoCT®, which is capable of obtaining a higher differentiation of the tissue margins and interphases, reaching a high definition of the lateral and lower margins. The surgical planning could be based on the measurement obtained through this technique. We have also used a second generation intravenous contrast (sonoVue®), consisting of microbubbles of sulfur hexafluoride mixed with sodium chloride 0.9%. Using this intravenous contrast, the intratumoral vascularization is highly enhanced. As an intratumoral vascularization is an accurate characteristic of melanoma angiogenesis, and it can be used to determine the high risk of melanoma metastasis development. Our patient had, with this technique, a prominent melanoma vascularization. The clinical evaluation of our patient was wrong, presenting left axillary lymph recurrence at six months of follow-up. He had bilateral pulmonary metastasis in the first year after the surgical removal of the melanoma. In a year and three months, it was found that he had cerebral metastases. In conclusion, the wrong clinical evaluation of our patient can be correlated with the prominent vascularization which was shown on sonography.
Differential Diagnosis List
Final Diagnosis
Melanocytic melanoma. A breslow index of 3.05 mm. Sentinel lymph node positive axilar left (HMB-45 positive).
Liscense
Figures
A sonograph of skin tumor
Color-Doppler revealing skin tumor

Enhanced color-Doppler with intravenous contrast agent

US Doppler spectrum

Throacic CT

Medical Imaging Analysis Report
1. Imaging Findings
Based on the ultrasound images (conventional ultrasound and color Doppler), an area of increased skin thickness on the back can be observed, presenting as a hypoechoic mass. The thickness of the mass is measured at approximately 3.55 mm. Color Doppler shows abundant blood flow signals within the lesion, along with noticeable intratumoral vascular enhancement (which became more prominent following the use of second-generation ultrasound contrast agents). This enhancement suggests a higher level of tumor angiogenesis.
In the chest CT images, nodular shadows can be seen in the lung fields. The arrow indicates a suspected metastatic lesion, which appears relatively small with well-defined margins—consistent with distant metastasis. Combining the postoperative follow-up findings, recurrence of the left axillary lymph nodes was confirmed, followed by evidence of bilateral pulmonary and brain metastases.
2. Potential Diagnoses
- Malignant Melanoma: Based on the tumor thickness (3.55 mm), abundant tumor angiogenesis, and the patient’s subsequent pulmonary and cerebral metastases, malignant melanoma is highly suspected.
- Benign Melanocytic Nevus: Although pigmented nevi are more common clinically, they typically have less vascularity compared to malignant melanoma and rarely develop distant metastases, which does not match the findings and disease course in this case.
- Other Skin Tumors (e.g., Pigmented Basal Cell Carcinoma, Squamous Cell Carcinoma, etc.): Certain pigmented variants of squamous cell carcinoma or basal cell carcinoma may show pigmentation; however, distant metastases and the high vascularity demonstrated by ultrasound are inconsistent with metastatic skin lesions deriving from other distant primary sites. Malignant melanoma features dominate in this scenario.
In summary, malignant melanoma best fits the patient’s clinical presentation.
3. Final Diagnosis
Considering the patient’s age, disease course, ultrasound and CT findings, and the subsequent development of axillary lymph node recurrence and metastases to the lungs and brain, the final diagnosis is malignant melanoma with distant metastases.
If further differentiation or therapeutic decision-making is needed, genetic testing (e.g., BRAF, NRAS) on the excised tissue may help guide the choice of targeted or immunotherapeutic strategies.
4. Treatment Plan and Rehabilitation Program
For malignant melanoma, treatment options primarily include surgery, immunotherapy, chemotherapy, and radiotherapy. Given a Breslow index of 3.55 mm, consideration should be given to surgical excision with a margin of approximately 3 cm, along with assessment or dissection of regional lymph nodes. In the event of distant metastases (e.g., lungs, brain), the following may be considered:
- Surgical Treatment: Wide local excision for early or resectable localized tumors; in cases with metastases, consider concurrent debulking or metastasectomy if feasible.
- Pharmacological Treatment:
- Immunotherapy: PD-1 or PD-L1 inhibitors (e.g., Nivolumab or Pembrolizumab) and/or CTLA-4 inhibitors (Ipilimumab).
- Targeted Therapy: In cases of confirmed BRAF mutations, BRAF inhibitors (e.g., Vemurafenib) combined with MEK inhibitors can be used.
- Chemotherapy: Traditional chemotherapy agents may be considered when immunotherapy is not tolerated or when no relevant targetable mutations are detected.
- Radiotherapy: Particularly effective for brain metastases or unresectable local lesions. Can be combined with immunotherapy or targeted therapy.
Rehabilitation/Exercise Prescription Recommendations:
In this case, the patient has already developed distant metastases, which may impair overall physical function. Therefore, an individualized and gradual rehabilitation and exercise program should be drawn up according to the patient’s general condition (especially cardiopulmonary reserve and musculoskeletal strength):
- Initial Phase (Postoperative/Early Treatment):
- Type of Exercise: Light walking, stationary cycling, or low-intensity water-based activities.
- Frequency: 3–4 times per week, 15–20 minutes per session, potentially split into 2–3 segments based on tolerance.
- Intensity: Maintain a slow pace or a mild sweat (heart rate <60% of maximum heart rate).
- Intermediate Phase (Disease Relatively Stable or Recovery):
- Type of Exercise: Moderate-intensity aerobic activities (e.g., brisk walking, mild uphill walking, or cycling), with the addition of mild resistance training.
- Frequency: 4–5 times per week, 20–30 minutes per session.
- Intensity: Gradually increase to 60%–70% of max heart rate, based on tolerance and cardiopulmonary function evaluations.
- Long-Term Phase (Maintenance or Long-Term Management):
- Type of Exercise: Combine aerobic and strength training, and include balance, core, and flexibility exercises as appropriate.
- Frequency: At least 5 times per week, integrating overall functional training with daily activities.
- Intensity: Adjust based on patient’s condition and subjective feedback. Ensure safety and schedule regular follow-ups.
- Special Considerations: If there is bone metastasis or fragile bones, avoid high-impact exercises or those placing significant load on the skeleton. In cases of poor cardiopulmonary function, exercise intensity and duration should be gradually increased under professional supervision.
Disclaimer
The above report is a reference analysis based on existing clinical and imaging information and does not carry legal authority for final diagnosis and treatment. Specific diagnosis, treatment, and rehabilitation plans must be determined by in-person consultations and comprehensive evaluations by qualified medical professionals.
Human Doctor Final Diagnosis
Melanocytic melanoma. A breslow index of 3.05 mm. Sentinel lymph node positive axilar left (HMB-45 positive).