Osteochondroma of thoracic spine presenting as upper limb radiculopathy



Clinical History
A case of 36 year old with an osteochondroma of T1 vertebra with cervical radiculopathy is reported. Osteochondromas comprise 36% of benign tumours of the bone. Osteochondromas of the spine commonly involve the posterior elements and may cause compressive myelopathy and/or radiculopathy.
Imaging Findings
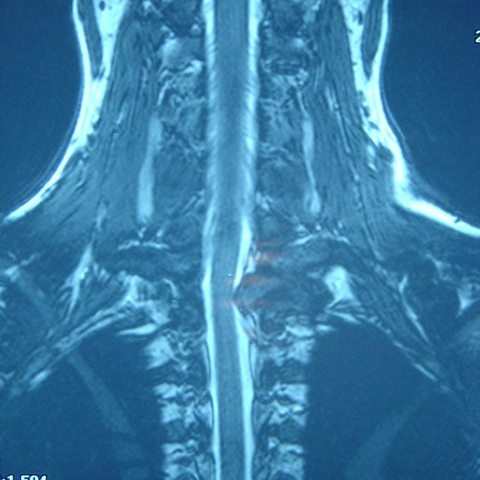
A 36 year old woman presented with stiffness in her neck, associated with radiating pain in her left upper limb, tingling and numbness in the 4th and 5th fingers of her left hand. She developed the symptoms following an injury to her neck, which she sustained in a road traffic accident 3 years ago. Her symptoms gradually increased in severity and were not relieved by anti inflammatory medication. On clinical examination, she was non-tender over the neck. All movements were terminally restricted with the exception of flexion. Diminished sensation in the left C8 and T1 dermatomes was the only positive neurological finding. Plain radiographs of cervical spine revealed a lesion at the level of T1 vertebra.(Fig.1). CT scan of the cervical spine showed a loculated tumour in the left pedicle and lamina of T1 vertebra (Fig. 2). MRI of cervical spine revealed an osseous mass originating from the left pedicle of T1 vertebra causing impingement of C8 and T1 nerve roots on the left side (Fig. 3).Technetium bone scan did not reveal any other skeletal lesions.The tumour was excised from the posterior elements of T1 vertebra by left sided hemi laminectomy and instrumented posterolateral fusion from C7 to T3 was performed, with no peri-operative complications (Fig. 4). At 2 years follow up the patient had complete relief of her symptoms. Histological examination of the submitted tumour was consistent with osteochondroma.
Discussion
Osteochondromas commonly involve long bones. It is unusual for an osteochondroma to originate in the vertebral column, the incidence being 1.3% to 4.1%1. They constitute 3.4% of all solitary spinal tumours1. Their incidence is slightly higher in patients with hereditary multiple exostoses (9%)1.The most common form of this mass is solitary and sporadic2. The less common form, the hereditary multiple exostoses, is a familial disease in which multiple osteochondromas are scattered in the axial or appendicular skeleton2. Spinal involvement with cord compression has been reported in 1% to 2.5% of patients with the hereditary form3, but cord compression is quite rare in the sporadic type of osteochondroma4,5. Osteochondromas have been encountered at all levels of the spine, but they have predilection for the cervical spine, particularly to the atlanto-axial region. Lesions most commonly arise from the posterior elements, although some originate from the vertebral body as well. Osteochondromas of the column may cause neurological symptoms as a consequence of their expansive growth into the spinal foramen or the involvement of the paravertebral sympathetic centers3,6. A palpable mass may be appreciated in those cases in which the lesions extend posteriorly, whereas dysphagia, hoarseness and vascular complications are more likely in osteochondromas that protrude anteriorly. Review of literature revealed 104 cases of spinal osteochondromas2,5,7,8,9. The solitary type was the most common (80 of 104). Of the 80 solitary osteochondromas, 41 cases presented as spinal cord compression. The average age was 40 years and male patients were more frequently affected. Patients with multiple exostoses tended to come for treatment at a younger age and had a much higher rate of spinal cord compression. In the current case the neural compression presented as radiculopathy. 23 cases (55 %) occurred in the cervical spine, 17 cases (41 %) in the thoracic spine and 2 cases (4 %) in the lumbar spine. The most frequent location in the thoracic spine was noted to be T8 (28%), followed by T4 (17%). On the plain radiographs, the osteochondroma appears as a calcified smooth mass composed of a cortex that is continuous with that of the underlying bone and spongiosa. At the point of attachment, the cortex of the bone of origin flares into the cortex of the osteochondroma7. Computerised tomography with thin sections and reconstructions demonstrates the typical findings of a benign osseous tumour with inner calcifications, in continuity with the rest of the bone8. It also defines the tumour’s extent and its relationship to the vertebrae and neural elements7. Because magnetic resonance imaging better defines the involvement of soft tissues and the bone marrow, it is the gold standard for evaluation of intraspinal expansion and spinal cord compression9. Conditions that could mimic this clinical presentation include cervical intervertebral disc herniation with root compression, thoracic outlet syndrome and cervical spondylosis with radiculopathy.
Differential Diagnosis List
Final Diagnosis
Histological examination of the submitted tumour was consistent with osteochondroma.
Liscense
Figures
AP View

CT Scan

MRI
Post operative AP View

Medical Imaging Analysis Report
I. Imaging Findings
Based on the provided X-ray, CT, and MRI images, a bony protrusion is observed in the upper cervical region (T1 vertebral body). Its density is comparable to that of normal bone, and the cortical bone appears continuous with the vertebral cortex. Thin-section CT scanning and reconstruction demonstrate that the cancellous portion of this outgrowth connects with the vertebral bone marrow, indicating a benign osseous growth. On MRI, there is evidence of compression on the dura sac and nerve root, consistent with cervical nerve root compression.
The overall shape presents as an exostosis with a relatively smooth outline and no significant soft tissue mass signal. There is no notable destructive or reactive change in the surrounding bone. These imaging findings suggest that this bony protrusion exerts a degree of compression on the adjacent nerve root, aligning with the clinical presentation of cervical nerve root irritation (cervical radiculopathy, radiating pain or numbness in the upper extremities, etc.).
II. Potential Diagnoses
-
Bony Protrusion (Osteochondroma)
Basis: The lesion is continuous with normal cortical bone, exhibits exophytic growth, and has well-defined margins. The patient’s age and symptoms are also consistent with this diagnosis. Although commonly found in long bones, osteochondromas that appear in the posterior aspect of the vertebra can cause spinal cord or nerve root compression. -
Degenerative Osteophyte (Bone Spur)
Basis: Degenerative osteophytes are often associated with disc or facet joint degeneration and can cause nerve root compression. However, they are usually smaller and located around the joint margins, and they typically do not show a continuous cancellous structure with the vertebral body on imaging. -
Other Intraspinal or Bony Lesions (e.g., Bone Island, Other Benign Vertebral Tumors)
Basis: Although less common, other benign tumors (such as bone islands or enchondromas) should be considered. Nonetheless, the X-ray and CT findings in this patient more characteristically match the typical imaging features of an osteochondroma.
III. Final Diagnosis
Taking into account the patient’s age, clinical symptoms (neck and shoulder/upper limb pain and numbness due to cervical nerve root compression), and imaging findings (a continuous bony outgrowth at the posterior aspect of the T1 vertebral body with both cortical and cancellous continuity, and evidence of nerve root compression), the most likely diagnosis is:
Cervical Vertebral Osteochondroma with Cervical Nerve Root Compression.
If doubts remain, further imaging post-processing or surgical pathology evaluation can be considered to obtain a definitive diagnosis.
IV. Treatment Plan and Rehabilitation Program
1. Overview of Treatment Strategies:
- Conservative Treatment: If symptoms are mild and neural function is not severely compromised, initial management may include physical therapy, analgesics, and anti-inflammatory medications. Regular observation is advised to monitor any progression of the lesion.
- Surgical Intervention: In cases of pronounced nerve compression symptoms (e.g., persistent pain, limb weakness, sensory deficits) or evidence that the lesion is enlarging, surgical resection of the outgrowth and decompression should be considered. Depending on the stability of the vertebra, internal fixation or fusion may be performed to prevent postoperative instability.
2. Rehabilitation Training and Exercise Prescription (FITT-VP Principle):
- Frequency: It is recommended to engage in rehabilitation activities 3–5 times per week to ensure gradual recovery.
- Intensity: Begin with low-intensity neck and shoulder movements and stretching exercises to avoid excessive rotation or load. Gradually increase muscle strengthening exercises in the mid to late stages according to symptom relief.
- Time: Start with 10–15 minutes per session and gradually extend to 30 minutes. If significant discomfort occurs, rest and adjustments should be made promptly.
- Type:
- Neck and Upper Back Stretching: Such as towel-assisted neck stretching, shoulder and neck stretches, or seated rowing with light resistance.
- Core Stability Exercises: For example, supine abdominal contractions or the “bird dog” exercise, which help maintain spinal stability.
- Cardiovascular Training: Low-impact aerobic exercise (such as brisk walking or using the elliptical machine) that does not place excessive stress on the cervical spine, helping to improve overall fitness.
- Progression: Gradually increase training intensity and duration according to pain relief and neurological recovery. If nerve symptoms worsen or new symptoms arise, discontinue training and seek medical attention promptly.
- Volume and Pattern: Keep each training session at a moderate volume, ensuring sufficient rest and recovery. Interval training methods can be used to avoid sustained high-intensity loads.
For patients with cervical instability or fragility, training should be performed under the protection of a cervical brace or professional supervision. Progress to higher-intensity or more complex movements only when it can be done safely.
Disclaimer:
This report is based on the current imaging data and clinical history, and it is intended for reference purposes only. It is not a substitute for an in-person consultation or the opinion of a qualified medical professional. If you experience any discomfort or have concerns, please seek prompt advice from a specialist.
Human Doctor Final Diagnosis
Histological examination of the submitted tumour was consistent with osteochondroma.