Four part proximal humeral fracture


Clinical History
Most proximal humeral fractures are minimally displaced or undisplaced and can be managed conservatively. Displaced fractures pose a treatment challenge and their successful management depends upon accurate plain radiographs, and CT and MRI scans as needed. Our patient had a likely 4-part fracture and required CT scan for better characterisation.
Imaging Findings
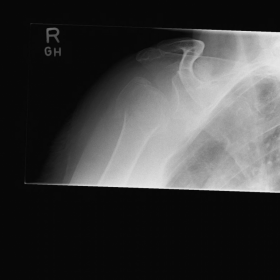
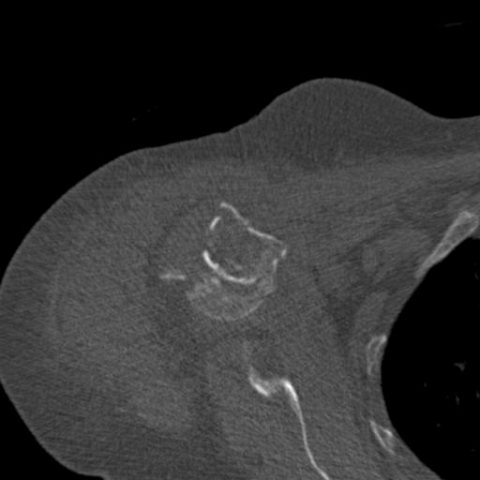
65-year-old lady was brought into the Emergency department after having sustained a fall by a swimming pool resulting in an injury to her right shoulder. Plain radiographs (Fig1) of the shoulder showed a likely four-part fracture of the proximal humerus. CT scan (Fig2) of the shoulder was performed for better characterisation of the fracture to plan further management. She underwent a hemiarthroplasty of the shoulder (Fig3) and made an uneventful recovery.
Discussion
Careful radiographic evaluation of patients with proximal humeral fractures is critical for accurate diagnosis and successful treatment.
Radiographic examination of the shoulder should include Neer's 1 trauma series, which consists of a true anteroposterior (AP) view of the glenohumeral joint, scapular lateral radiographs ‘y-view’, and axillary view.
In the Neer1 classification of proximal humerus fractures, the proximal humerus is made up of four parts:
1. humeral head (articular surface)
2. greater tubercle
3. lesser tubercle
4. diaphysis (shaft)
These four parts are separated by epiphyseal lines (bone growth plates) during the early developmental years. When the proximal humerus is broken, the fracture line predictably occurs along one or more of these planes.
Displacement of a fracture fragment by 1 cm, or angulation between fracture fragments of 45° or greater, is what defines a fragment as being a "separate" part. Hence, a proximal humerus fractures may be called 2-part, 3-part, or 4-part according to the Neer classification system, depending upon the amount of displacement and angulation seen on plain radiographs
Sometimes it is difficult to see the exact position of the fracture fragments, or the patient may be difficult to position. Kristiansen et al. found wide interobserver variation in the classification of proximal humeral fractures when only plain radiographs were used2. Accuracy of assessment improved with more experience in the use of the Neer classification. Studies3 show that CT can be useful in difficult cases where the amount if displacement or rotation of fragments is difficult to determine on plain radiographs.
Operative treatment includes closed reduction with percutaneous fixation, open reduction and internal fixation, and proximal humeral head replacement4. Fracture patterns best suited for arthroplasty of proximal humerus fractures have been 4-part fractures, fracture dislocations, head-splitting fractures, impaction fractures, humeral head fractures with involvement of more than 50% of the articular surface, and 3-part fractures in elderly patients with osteoporotic bone. However, within these groups, heterogeneity of fracture patterns exists.
Differential Diagnosis List
Final Diagnosis
Four part proximal humeral fracture
Liscense
Figures
Plain radiograph



CT scan with 3D reconstruction



Post hemiarthroplasty check radiograph

1. Radiological Findings
Based on the provided anteroposterior (AP), Y-view, and axial X-ray images of the shoulder, as well as subsequent cross-sectional and 3D reconstructed CT images of the upper arm, multiple fracture lines are observed in the proximal right humerus, involving the humeral head, the area between the tubercles (intertubercular region), the greater and lesser tubercles, and the proximal humeral shaft. Some fracture lines show obvious displacement and separation, along with a noticeable change in angulation.
In the postoperative images (the last X-ray), an artificial humeral head or proximal humeral prosthesis can be seen, indicating that a shoulder joint or proximal humeral prosthetic replacement was performed during surgery. The implanted prosthesis within the fracture area appears to be in a generally good position.
2. Potential Diagnoses
- Proximal Humerus Four-Part Fracture (Neer Four-Part Fracture):
Previous literature and examinations demonstrate that the fractures around the proximal humerus follow anatomical structures (the greater tubercle, lesser tubercle, the humeral shaft, and humeral head) and involve at least four segments with marked displacement and/or angulation, characteristic of a classic four-part fracture. - Proximal Humerus Three-Part Fracture:
In a few patients, if the angulation on shoulder X-rays is not very obvious, or if only significant separation of the greater and lesser tubercles from the humeral head is present while humeral shaft displacement is minimal, a three-part fracture could be considered. However, based on the CT findings (displacement and angulation), a four-part fracture is still more likely. - Other Shoulder Injuries or Old Fractures:
If there is a history or clinical symptoms suggesting chronic pain, one should exclude old fractures or worsening osteoporotic fractures. Nonetheless, the imaging reveals clear signs of a fresh fracture, indicating an acute fracture, making these possibilities less likely.
3. Final Diagnosis
Taking into account the patient’s age (65 years old, female), clinical presentation (severe shoulder pain and restricted movement after trauma), imaging features (multiple fracture lines in the proximal humerus with at least four distinct segments showing obvious displacement or angulation), and the postoperative imaging that indicates shoulder prosthesis replacement, the most likely final diagnosis is:
Right Proximal Humerus Four-Part Fracture (Neer Four-Part)
4. Treatment Plan and Rehabilitation
4.1 Overview of Treatment Strategy
In elderly patients with a four-part proximal humerus fracture, if there is severe displacement, joint surface damage, or a high risk of avascular necrosis, surgical intervention is often necessary, such as:
- Open Reduction and Internal Fixation (ORIF): Indicated for local or less displaced fractures. In cases of sufficiently strong bone quality, fixation with plates, screws, or intramedullary nails may be used.
- Joint Prosthetic Replacement (Shoulder Arthroplasty/Proximal Humerus Prosthesis): When osteoporosis is severe, the blood supply to the humeral head is significantly compromised, or the fracture is highly comminuted, prosthetic replacement may be considered to restore shoulder function more quickly.
Given that the final imaging shows prosthetic replacement, this patient has undergone a shoulder prosthesis procedure. Postoperative management should focus on functional rehabilitation to minimize joint stiffness and soft tissue atrophy.
4.2 Rehabilitation/Exercise Prescription Suggestions (FITT-VP Principle)
The following rehabilitation plan should be carried out under the guidance of a qualified rehabilitation physician or physical therapist, tailored to the patient’s individual conditions (bone quality, level of postoperative pain, cardiopulmonary function, etc.), and progressed gradually:
- F (Frequency): In the early stage (within 2–4 weeks post-surgery), perform passive exercises 2–3 times a day. In the mid to late stage (4–8 weeks post-surgery), reduce to 1–2 times a day and gradually increase the proportion of active exercises.
- I (Intensity): Begin mainly with passive movements and assisted active movements, avoiding significant pain. As fracture healing and pain relief improve, gradually introduce light resistance exercises for muscles like the biceps, triceps, and deltoid.
- T (Time): Each session may last about 10–20 minutes, done in sets. As tolerance grows, each session can be extended to 20–30 minutes.
- T (Type): Focus on range of motion exercises, shoulder pendulum exercises (including the pendulum swing), joint mobilization techniques, and muscle strengthening. Gradually introduce resistance bands or light weights in the later stages.
- V (Volume): Increase total training volume gradually according to patient tolerance and pain levels, aiming for at least 5–7 sessions of shoulder exercises per week. After each session, allow rest and consider intermittent ice packs or pain management strategies.
- P (Progression): Progressively adjust rehabilitation by increasing the range of motion, adding resistance, or extending exercise duration. After the patient can manage essential daily activities, continue to advance toward normal shoulder function.
During the fracture healing phase and postoperative rehabilitation, ensure that areas of weakened bone are not exposed to excessive stress and avoid falls or heavy loads. Monitor shoulder and upper limb pain and swelling, and seek timely follow-up and evaluation as needed.
Disclaimer: This report is a reference analysis based on the provided clinical history and imaging data. It does not replace an in-person consultation or the opinion of a qualified medical professional. If you have any concerns or changes in your condition, please consult a specialist promptly and follow their recommendations for further evaluation and treatment.
Human Doctor Final Diagnosis
Four part proximal humeral fracture