Intraarticular nodular fasciitis of the knee



Clinical History
A 47-year-old man presented in the orthopaedics department with right knee pain of 4 months duration, preferably in the posterior aspect of the joint. There was no history of trauma.
At the physical examination, the meniscus manoeuvres and pivot shift test were negative, and there were no palpable masses.
Imaging Findings
Conventional radiographs did not show any abnormality. Bone density and joint space were preserved.
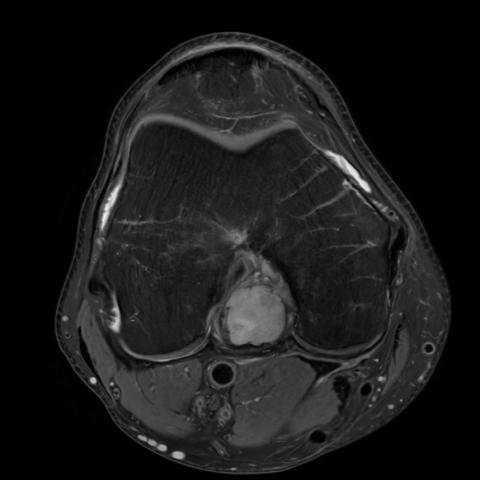
The Magnetic Resonance Imaging (MRI) of the right knee showed a solid nodular lesion in the posterior intercondylar region, just posterior to the posterior cruciate ligament. The lesion presented well-defined margin with lobulated shape and measured 1,8 x 2 x 3,3 cm.
It was predominantly hyperintense compared to surrounding muscle on Proton Density (PD) weighted images, with and without fat suppression (FS) technique.
Minimal joint effusion was also shown.
The MRI was performed without intravenous contrast, because the patient refused to use it.
The diagnoses suggested by the radiologist after the MRI were focal synovitis and pigmented villonodular synovitis.
Due to the finding, the orthopaedic surgeons decided to undergo arthroscopic surgery to excise the lesion.
The postoperative radiological study was performed 6 months after the surgery, and it does not show any residual or new lesion.
Discussion
Background
Nodular fasciitis is a self-limiting benign lesion characterized by a myofibroblastic proliferation in patients between 20 and 50 years old [2]. It usually appears as a palpable mass in the subcutaneous tissues and attached to the fascia [5].
Intraarticular nodular fasciitis is rarely reported and only 21 cases have been documented in the literature (3).
Clinical Perspective
Most of the patients with intraarticular nodular fasciitis presented with painful joint, limited range of motion, palpable masses, joint effusion or hemarthrosis. 15% of the patients had history of previous trauma before the diagnosis [2]. The duration of symptoms before surgical excision ranged from 1 month to 1 year [3]. Intra-articular nodular fasciitis tended to have a longer preoperative history than the usual variants [2].
The knee was the most common joint affected (70%) followed by the shoulder, the hand, the hip and the elbow [1].
Imaging Perspective
The conventional X-ray of the painful joint is usually normal. The MRI is the best imagine technique for characterize and detect intraarticular nodular fasciitis [3].
In the MRI the disease usually presents as a circumscribed lesion ranged from 1 to 6 cm [3]. The T1-weighted MRI shows iso-signal intensity compared to the surrounding muscle, while the T2-weighted MRI and the DP-weighted MRI showed high signal [3].
Contrary to subcutaneous nodular fasciitis, in the intraarticular form could show magnetic susceptibility artifacts in gradient echo sequences, as pigmented villonodular synovitis does [2].
Post-gadolinium-enhanced imaging demonstrated diffuse, slightly inhomogeneous T1-weighted enhancement of the nodular lesions [5].
Outcome
As intraarticular nodular fasciitis is rarely encountered, it is commonly misdiagnosed, and most cases are thought to be intraarticular diseases with higher incidence rate such us: pigmented villonodular synovitis, synovial chondromatosis, desmoid-type fibromatosis or giant cell tumour of tendon sheath [1].
Although intraarticular nodular fasciitis usually regress spontaneously and it does not recur in the follow up, almost all the patients reported in the literature underwent arthroscopic surgery to excise the lesion.
The diagnosis must be confirmed by the anatomopathological study, where the lesion shows typical histologic features of nodular fasciitis: unencapsulated and well-circumscribed lesions composed of uniform spindle cells in bundles with vesicular chromatin, small nucleoli, and eosinophilic cytoplasm, no significant cytologic atypia or pleomorphism. Contrary to conventional variants of nodular fasciitis, it is common for the intraarticular form to find prominent stromal hyalinization, cystic degeneration and hemosiderin deposition, because of the repeated frictional trauma due to the anatomic localization [1].
After surgery, symptoms relieved in a few days [3].
Take Home Message / Teaching Points
Nodular fasciitis should be included in the differential diagnosis for any intraarticular mass lesions. Although MRI is useful to characterize the lesion, histological examination is essential to establish the diagnosis.
Differential Diagnosis List
Final Diagnosis
Intraarticular nodular fasciitis of the knee
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures



Medical Imaging Analysis Report
1. Imaging Findings
The patient is a 47-year-old male complaining of right knee pain for 4 months without any significant history of trauma. The knee MRI sequences (including T1-weighted, T2-weighted, PD-weighted images, etc.) demonstrate the following:
- A relatively well-defined nodular soft tissue lesion is observed in the posterior portion of the joint cavity (adjacent to the joint capsule or nearby structures).
- On T1-weighted images (T1WI), the signal is similar to that of surrounding muscle (isointense or slightly hypointense). On T2-weighted images (T2WI) and PD-weighted images, it appears hyperintense, indicating relatively high water or fluid content within the lesion.
- After contrast administration, the lesion exhibits mild to moderate heterogeneous enhancement with a slightly inhomogeneous distribution.
- No signs of fracture or bone marrow edema are observed in the surrounding bone, and there is no extensive infiltration or destruction of adjacent soft tissues. No significant synovial proliferation or diffuse changes are noted in the local synovium.
In summary, the MRI suggests a circular or oval soft tissue lesion within the joint with benign characteristics, and there is no evidence of invasion into bone or destruction of adjacent soft tissues.
2. Potential Diagnoses
Based on the patient’s clinical presentation (middle-aged male, chronic joint pain, no history of trauma) and imaging findings (intra-articular focal soft tissue lesion with well-defined margins, T2 hyperintensity, and mild heterogeneous enhancement post-contrast), the following potential diagnoses are considered:
- Intraarticular Nodular Fasciitis
- Characteristics: A benign lesion caused by fibroblastic or myofibroblastic proliferation. It can occur in subcutaneous or deeper tissues, but intraarticular occurrences are extremely rare.
- Imaging: Typically presents as a soft tissue mass within the joint, with hyperintensity on T2WI, possible mild to moderate enhancement, and relatively well-defined margins.
- Pigmented Villonodular Synovitis (PVNS)
- Characteristics: Synovial proliferation with hemosiderin deposition, often presenting with joint pain and effusion. On MRI, areas of “T2 low signal” may be seen, and gradient echo sequences often show susceptibility artifacts.
- In this case, while minimal susceptibility-related changes are possible, the lesion’s overall morphology is more indicative of a localized nodule rather than a diffuse synovial process.
- Synovial Chondromatosis
- Characteristics: Formation of cartilaginous nodules within the synovium, often accompanied by multiple calcifications on imaging. On MRI, multiple small nodules with local calcification are commonly seen within the joint.
- No obvious calcifications or multiple nodules are observed in this case, making this diagnosis less likely.
- Desmoid-type Fibromatosis
- Characteristics: Locally aggressive. On MRI, it can present with heterogeneous signals, and the lesion margins are often less well-defined than benign lesions.
- Here, only a focal nodule is noted, with no evident destruction of surrounding structures, making this diagnosis less probable.
- Giant Cell Tumor of Tendon Sheath
- Characteristics: Typically located near tendon sheaths or synovium, presenting as a well-defined soft tissue nodule that may have hemosiderin deposition.
- In this case, the lesion is intra-articular and appears relatively homogeneous with T2 hyperintensity, which does not fully align with the common characteristics of giant cell tumor of tendon sheath.
3. Final Diagnosis
Considering the patient’s age (47), symptoms (chronic knee pain, unremarkable physical examination, no palpable mass), imaging findings (a localized soft tissue nodule in the joint with T1 isointensity, T2 hyperintensity, mild to moderate enhancement post-contrast, absence of significant synovial proliferation or multiple calcifications, and lack of bony involvement), and the rarity yet similarity of reported cases, the most likely diagnosis is:
Intraarticular Nodular Fasciitis.
If feasible, arthroscopic exploration and surgical excision of the lesion for pathological examination can be undertaken to confirm the diagnosis and exclude other rare intra-articular conditions.
4. Treatment Plan and Rehabilitation
For intraarticular nodular fasciitis, the main treatment approaches may include:
- Arthroscopic Surgical Excision: Many case reports indicate successful removal of the lesion under arthroscopy. This method is suitable for patients with significant symptoms, larger lesions, or uncertain diagnoses.
- Conservative Observation: Because the condition may be self-limiting, if symptoms are mild, regular monitoring and follow-up imaging may be sufficient. Some lesions can resolve spontaneously.
After arthroscopic excision or during conservative management, individualized rehabilitation exercises can be implemented. Rehabilitation and exercise prescriptions can be divided into stages:
- Acute Phase (early post-operative period or severe symptoms)
- Training Goals: Reduce pain and swelling, restore basic joint range of motion.
- Recommended Methods: Combine active and passive joint movements, avoiding excessive weight-bearing. Gentle flexion and extension exercises in a seated or supine position 2-3 times per day, 5-10 minutes each session.
- Recovery Phase
- Training Goals: Gradually increase joint range of motion and strengthen periarticular muscles.
- Recommended Methods: Begin low-intensity resistance exercises (e.g., resistance bands) 3 times per week, 15-20 minutes each time, combined with exercises such as wall squats or seated leg presses, starting from light to moderate loads.
- Strengthening Phase
- Training Goals: Restore and improve joint proprioception and stability, returning to normal functional activities.
- Recommended Methods: Low-intensity jumping drills, balance training (e.g., balance board), closed-chain strength exercises, and proprioceptive training 3-4 times per week, about 30 minutes per session.
- Maintenance Phase
- Training Goals: Maintain recovery gains and prevent recurrence.
- Recommended Methods: Engage in regular moderate strength and joint flexibility exercises, such as swimming or cycling (low-impact aerobic activities), 2-3 times per week.
Throughout the rehabilitation process, it is crucial to adhere to the individualized, progressive FITT-VP principle (Frequency, Intensity, Time, Type, Progression, Volume) and make adjustments based on the patient’s subjective symptoms, joint swelling, and pain level. If pain or swelling worsens, reduce exercise volume and seek medical advice promptly.
Disclaimer: This report is based on the preliminary analysis of limited clinical and imaging data, serving as a reference only. It does not replace an in-person consultation or professional medical advice. The specific treatment plan should be determined in conjunction with clinical evaluations, surgical findings, and pathological results. If you have any questions or changes in your symptoms, please consult a physician promptly.
Human Doctor Final Diagnosis
Intraarticular nodular fasciitis of the knee