Septic arthritis



Clinical History
52 year old male presented at the emergency department because of inability to walk.
Imaging Findings
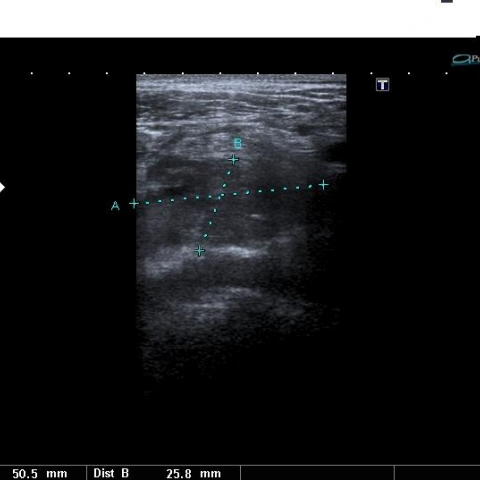
A 52 year old male patient came to the emergency department becasue of inability to walk. His medical history was unremarkable and physical examination revealed restricted mobility of his right leg. The first radiographs (Fig. 1) and the laboratory test were normal, so he went home. After 20 days the patient came again to the ER and new radiographs (Fig. 2) revealed a destruction of the right femoral head. A superficial venous thrombosis and an abscess were found on ultrasonography (Fig. 3). A MR of the right femoral head and iliac bone showed low signal intensity of the lesion on T1-WI and high signal intensity on PD-WI with fat saturation (Fig. 4). A MNGA (Fig. 5) studie was performed, showing a tracer hyperfixation at the right femoral head. Staphylococcus aureus was found in the aspirated synovial fluid.
Discussion
Septic arthritis is a common, often disabling disease that requires early diagnosis for optimal outcome. Diagnosing septic arthritis early in its course is important because delayed diagnosis may result in cartilage and joint destruction arising from the action of enzymes released from neutrophils, synovial cells, and bacteria. Septic arthritis is traditionally a clinical diagnosis based on physical examination and prompt arthrocentesis. The paucity of specific clinical findings at the time of presentation has been noted. Septic hip is diagnosed when effusion, loss of cartilage, and cortical bone destruction are present. The cartilage loss will not be seen in early septic hips, and the radiographic findings may then be extremely subtle. Hip effusion will be detected by paying careful attention to the fat pads, with a side-to-side comparison. Early cortical bone loss or a decrease in cortical “distinctness” should be sought both on the acetabulum and the femoral head. The diagnosis must be secured by means of hip aspiration and culture of the aspirate. It is important to note that aspiration of a suspected septic hip is one of the true orthopedic emergencies encountered by radiologists. Delay in aspiration and treatment results in rapid destruction of the hip joint.
MRI has been increasingly used to evaluate musculoskeletal infections because it is useful for evaluating bone marrow, soft tissues, and joints. MRI findings in patients with septic joints have been described as abnormal as early as 24 hrs after the onset of infection. The sensitivity and specificity of gadopentetate dimeglumine– enhanced MRI with fat suppression were found to be 100% and 77%, respectively, for the detection of septic arthritis.
Differential Diagnosis List
Final Diagnosis
Septic arthritis
Liscense
Figures
Normal Rx right hip

Subtle indistinctnes of the cortical line of the right femoral head

Soft-tissue abscess next to the right femoral head.
Low signal intensity of the lesion on T1-WI

High signal of the right femoral head (Coronal fat sat)

MNGA: Tracer hyperfixation at the right femoral head

Medical Imaging Analysis Report
I. Imaging Findings
1. X-ray Plain Film:
- Pelvic AP view and bilateral hip X-rays show abnormal configuration of the joint space on the affected side (suspected left hip), with possible minimal effusion indicated by local soft tissue shadows; there is no prominent cartilage destruction yet, but early changes should be monitored.
- The cortical edge of the acetabulum or femoral head on the affected side appears faint and blurred, suggesting possible early cortical bone erosion.
- Compared with the contralateral hip joint, subtle changes in pericapsular space and fat lines are noted on the affected side, indicating potential joint effusion.
2. Ultrasound:
- Ultrasound imaging reveals a pronounced anechoic or hypoechoic region at the joint surface, measuring approximately 25.8 mm (in A–B dimension), suggesting intra-articular effusion or exudate.
- The surrounding soft tissue shows increased or disorganized echogenicity, further indicating possible acute inflammation or infection.
3. MRI:
- There is a conspicuous T2 hyperintense signal around the hip joint, indicating an accumulation of fluid in the joint space.
- Possible bone marrow edema of the femoral head and acetabular side, evident as T2 hyperintensity, suggesting an early response to bone or cartilage destruction.
- On contrast-enhanced sequences (if performed), enhancement of the joint capsule, synovium, and surrounding soft tissues can be seen, consistent with infection or acute inflammatory changes.
4. Bone Scan:
- The affected hip joint shows increased uptake of the radioactive tracer, suggesting inflammation, infection, or other high-metabolic processes.
- Based on a combination of clinical and imaging findings, infectious arthritis (particularly purulent/septic arthritis) is highly suspected.
II. Potential Diagnoses
- Purulent/Septic Arthritis
- The patient presents with acute hip pain and difficulty in ambulation.
- Imaging findings include joint effusion, early signs of bone destruction, and increased uptake on bone scan.
- Clinically, fever and elevated inflammatory markers (e.g., WBC, CRP, ESR) are common; joint aspiration often yields purulent fluid or positive pathogen culture.
- Acute Synovitis or Inflammatory Joint Disease
- May also present with joint effusion, though bone destruction is typically less prominent, and it often occurs in the context of specific autoimmune or rheumatoid diseases.
- MRI may show synovial thickening, but the degree of enhancement and bone marrow edema is usually relatively milder.
- Avascular Necrosis of the Femoral Head (Early Stage)
- Also presents with hip pain and limited function;
- However, MRI usually reveals a characteristic “double line sign” or other necrotic features, and the acute purulent signal is less common.
- Other Joint Conditions (e.g., Osteoarthritis, Post-traumatic Arthritis)
- In older patients, joint space narrowing, subchondral sclerosis, or cystic changes may be observed, but an acute rapid onset with significant effusion and marked inflammation is less typical.
III. Most Likely Final Diagnosis
Based on the patient’s clinical presentation (inability to walk, acute onset), likely elevated inflammatory markers, and the imaging findings (joint swelling, synovial thickening, bone marrow edema, joint effusion, early cortical erosion), the most probable diagnosis is Septic Arthritis of the Hip.
To confirm the diagnosis, joint aspiration and analysis (including Gram stain, culture, and sensitivity testing) along with serum inflammatory markers are essential.
IV. Treatment and Rehabilitation Plan
1. Treatment Strategy:
- Antibiotic Therapy: Choose antibiotics according to culture results from aspirated fluid and blood cultures; aggressive early anti-infective treatment is crucial.
- Joint Drainage or Lavage: If there is a large amount of effusion or suspected pus, arthroscopic or surgical drainage is indicated to reduce joint destruction.
- Symptomatic and Supportive Care: Includes analgesics, maintenance of fluid and electrolyte balance, and immobilization if necessary.
- Dynamic Assessment: Regularly monitor inflammatory markers (WBC, CRP, ESR) and clinical symptoms; imaging should be repeated to evaluate treatment efficacy.
2. Rehabilitation and Exercise Prescription (FITT-VP Principles):
During the acute phase, priority is rest and immobilization. As the condition stabilizes, progressively introduce rehabilitation exercises:
- Frequency: Initially 2–3 sessions per week; can increase to 3–5 sessions per week once symptoms improve.
- Intensity: Begin with low-intensity activities such as passive movement or low-resistance exercises, avoiding exacerbation of pain.
- Time: Start with 10–15 minutes per session, gradually increasing to 20–30 minutes based on tolerance.
- Type: Early stages may focus on gentle range-of-motion exercises (e.g., straight leg raises, passive hip movement). Progress later to water-based exercises or cycling with minimal impact.
- Progression: As joint pain decreases and strength improves, gradually increase range of motion, introduce light weight-bearing (e.g., using crutches transitioning to walking unaided), and add core strengthening and lower-limb functional training.
- Precautions:
1) In patients with frail bones or comorbidities, carefully control exercise intensity to avoid secondary injury.
2) Any exercise that causes sudden severe pain or swelling should be stopped immediately, and the plan should be adjusted in consultation with a physician or rehabilitation therapist.
V. Disclaimer
This report is based on the current imaging and clinical information for reference only. It cannot substitute an in-person consultation or the clinical diagnosis and treatment by healthcare professionals. In case of any doubts or changes in the patient’s condition, please consult a professional healthcare provider promptly for further evaluation and management.
Human Doctor Final Diagnosis
Septic arthritis