Aneurysmal bone cyst of the humerus: a report of a case resolved by a single embolization


Clinical History
Aneurysmal bone cyst is a benign, osteolytic, hyperplastic, hyperemic-hemorrhagic locally aggressive lesion mostly commune in children and young adults. Today’s therapy is selective arterial embolization or alternatively curettage and bone grafting. Embolization can have two aims: as preparation to surgery in order to decrease intraoperative bleeding risk or curative.
Imaging Findings
A 16-year-old Caucasian boy was referred to our department because of a pathologic fracture complicating an osteolytic lesion located on the proximal third of the right humerus discovered a month earlier during an X-ray performed for local pain and swelling.
There was no history of congenital or acquired bone pathology. There was no dysmetria of the upper limbs and no general symptoms such as fever, body weight and appetite lost. Pain increased through palpation; there were no ecchymosis or bruising. Systemic exams and laboratory studies were negative.
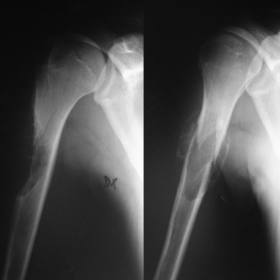
X-rays showed an eccentric osteolytic lesion with destruction of the lateral cortex at the proximal third of right humerus with local bump; a partially calcified hematoma was already present (fig.1); the aspect was highly suggestive of aneurysmal bone cyst (ABC). MRI showed a non-homogeneous lesion with internal septation (fig.2). Specific differential diagnosis was telangiectatic osteosarcoma. Bone scan indicated local uptake and absence of bone metastasis.
A needle biopsy was performed to exclude every malignancy and the clinical suspect was histologically confirmed.
A first embolization procedure was attempted and X-ray, performed after one month, showed a beginning of calcification process (fig.3); the last control, performed 10 months after the procedure, evidenced the healing of the ABC without the need of further procedures (fig. 4).
Discussion
ABC in not a neoplasm but his aspect can be similar to other locally aggressive or malignant lesions. The most common sites are the methaphysis or meta-diaphysis of the long bones of the lower limb then of the upper limb, spine and pelvis but severalbones can be involved. Pain and swelling are principal symptoms; nevertheless the clinical presentation depends on ABC localization [1].
X-ray usually shows an osteolytic, usually eccentric lesion with the cortex thinned or destroyed. There is a periosteum reaction and a slight reactive bone sclerosis can demarcate the lesion. The aspect is confirmed by CT scan showing single or multiple fluid levels due to a blood-serum division[1].
MRI shows internal septation with “soap-bubble” features particularly evident in T2 weight images with an enhancement of the septa after gadolinium infusion. When present a fluid level is characteristic; on in T1 weight images ABC has intermediate or low signal.
Differential diagnosis includes telangiectatic osteosarcoma, simple bone cyst and giant cell tumor therefore biopsy is preferable for diagnosis.
Telangiectatic osteosarcoma rarely may present like an aggressive ABC and the fluid-fluid levels can be present; also histology can be not clear in rare cases of low-grade telangiectatic osteosarcoma.
Simple bone cyst sometime may mimic an aneurysmal central bone cyst. The puncture in simple bone cyst evidences a clear fluid instead of blood in ABC. CT and MRI show a unicameral lesion in simple bone cyst.
Usually Giant cell tumor arises in patient over 20-years old so that the most of giant-cell-tumor-like lesions near to an open growth plate is an ABC. Differential diagnosis can be difficult in the adults because of giant cells can be present in ABC as well [1].
The treatment approach varies depending on the location and aggressiveness of the lesion. In quiescent form follow-up is possible; in aggressive, surgery is the most used treatment consisting in curettage with effective adjuvant therapy and bone grafting but high recurrence rate was reported [2-4].
Nevertheless when surgical approach is difficult and very invasive such as in ABC located in spinal and pelvic bone, embolization may be the best option [5,6]. The results obtained by embolization encourage the use of this method as first choice also in “easy approached lesions” both therapeutic or as preparation to surgery [7]. Today embolization is principal approach to ABC; surgery is necessary when embolization gives no results and as first choice when there is a high risk of fracture. Although in most cases several embolizations are necessary to allow healing ABC, sometimes a single procedure can be enough. Radiologists and orthopedics have to follow the healing process in order to postdate a possible second procedure. As a matter of fact if a good evolution is evident at X-ray useless procedure should be avoided and to assure the least invasive and efficient treatment.
Differential Diagnosis List
Final Diagnosis
aneurysmal bone cyst
Liscense
Figures
Radiography

Radiography

Radiography

No title

1. Imaging Findings
From the provided proximal humerus X-ray and MRI images, there is an eccentric, expansile bone lesion in the proximal humeral metaphysis or metaphyseal-diaphyseal junction. Specific findings include:
- On the X-ray: The lesion shows obvious lytic change, with thinning or local destruction of the cortex. The overall appearance is a “blow-out” expansion, and some “soap-bubble” septations may be seen.
- On MRI: On T2-weighted sequences, there are multi-chambered, fluid-fluid levels; the lesion is divided by multiple septa with high signal intensity. T1-weighted sequences generally show intermediate to low signal, with enhancement of septa and the lesion walls after contrast administration.
- No obvious extensive soft tissue infiltration surrounding the humerus is identified, and there are no clear signs of pathological fracture. However, due to cortical thinning, there is a potential risk of fracture.
2. Potential Diagnoses
Based on the patient’s age (16 years), clinical symptoms (pain and local swelling), and imaging findings (multi-chambered “soap-bubble” lytic lesion, fluid-fluid levels, etc.), the following differential diagnoses should be considered:
- Aneurysmal Bone Cyst (ABC):
- Common in adolescents. Typical X-ray findings include eccentric, expansile, septated lytic destruction, and on MRI, fluid-fluid levels may be observed.
- These features match the patient’s presentation, especially the “soap-bubble” appearance and fluid-fluid levels.
- Giant Cell Tumor (GCT):
- Common in the 20-40 age group, typically involving the epiphysis extending to the metaphysis, often after epiphyseal closure.
- Although it also shows lytic and septated changes on imaging, this patient’s age (16 years) and the lesion’s proximity to the growth plate make GCT less likely.
- Telangiectatic Osteosarcoma:
- Can present as a highly erosive lytic lesion with fluid-fluid levels, but usually displays more aggressive imaging features, such as extensive soft tissue involvement, tumor bone formation, or pronounced periosteal reaction.
- This possibility should be cautiously ruled out before combining imaging and clinical data with pathology, but it is relatively less likely.
- Simple Bone Cyst:
- Also common in adolescents, but typically presents as a unilocular cyst containing clear or straw-colored fluid rather than blood.
- On MRI, it usually appears as a single cyst, with fewer obvious septations or fluid-fluid levels.
3. Final Diagnosis
Considering the patient’s age, clinical symptoms, multi-chambered expansile bone destruction, fluid-fluid levels, and characteristic “soap-bubble” appearance on imaging, the most likely diagnosis is:
Aneurysmal Bone Cyst (ABC).
If there are any special changes in subsequent clinical or imaging follow-ups or if there is any diagnostic uncertainty, further biopsy or pathological examination may be considered for confirmation.
4. Treatment Plan and Rehabilitation
4.1 Treatment Strategy
For aneurysmal bone cysts, the general treatment principles include:
- Selective Arterial Embolization (SAE): Used as a primary or adjunct therapy to reduce bleeding and lesion size, especially useful for lesions located in areas where surgery is high risk or difficult to access.
- Curettage and Bone Grafting: For lesions that are easily accessible and show significant structural destruction, surgical curettage may be considered, followed by bone grafting or other internal fixation methods to reduce the risk of pathological fracture.
- Regular Follow-up: For relatively stable lesions, mild symptoms, or those with a trend of spontaneous healing after embolization, periodic imaging follow-up may be chosen.
4.2 Rehabilitation/Exercise Prescription Recommendations
Once the lesion is stabilized or after ensuring the skeletal structure is safe postoperatively, progressive functional recovery and exercise training should be implemented. Following the FITT-VP principle (Frequency, Intensity, Time, Type, Progression, and Volume):
- Frequency: Target 3-4 sessions of specialized rehabilitation training per week.
- Intensity: Begin with mild to moderate exercises, such as basic range-of-motion (ROM) activities, avoiding excessive stress on the affected limb.
- Time: 20-30 minutes per session, gradually increasing as tolerated.
- Type:
- Early Stage: Emphasize static and passive exercises, then gradually increase active joint mobility training.
- Intermediate Stage: Under the supervision of a professional rehabilitation therapist, introduce light resistance training, such as elastic band exercises, to improve upper limb strength and stability.
- Late Stage: If bone healing is satisfactory, gradually resume light weight-bearing activities and daily functional training.
- Progression:
- Increase training intensity and duration progressively based on treatment outcomes and X-ray follow-up findings.
- If there is pain or new discomfort, promptly evaluate and adjust the plan.
During the rehabilitation process, local pain, swelling, and changes in joint mobility should be closely monitored. If significant pain intensifies, the risk of fracture increases, or if there is fatigue and other symptoms, promptly return for a follow-up and coordinate assessment with the orthopedic and rehabilitation departments.
Disclaimer
This report is based on the currently provided medical history and imaging findings for reference only. It cannot replace in-person consultation or professional medical advice. Please follow the guidance of clinical specialists for specific diagnosis and treatment.
Human Doctor Final Diagnosis
aneurysmal bone cyst