

The patient presented with metatarsalgia. There was no history of trauma and X-ray was negative.
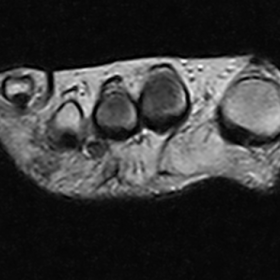
Sonography showed a hypointense area between the third and the fourth metatarsal heads; MRI study showed a hypointense area in the same region.
This was compatible with Morton's neuroma.
The patient, a 30-year-old man, presented with metatarsalgia, lasting for several months. There was no previous history of direct trauma.
Radiography of the affected foot (right foot) was negative.
The patient underwent an ultrasonography of the right foot which showed a hypoechoic small region between the third and the fourth metatarsal heads. A MRI study was performed in order to define the lesion. A 0,31 T dedicated MRI scanner was used, specific for the examination of the distal joints. The MR imaging protocol included a FSE T2 and a STIR sequence in the axial and coronal planes.
The T2 sequence showed a small hypointense area between the third and the fourth metatarsal heads compatible with Morton's neuroma. The STIR sequence showed a hyperintense region around the lesion as sign of bursitis.
Morton’s syndrome is a neuralgic metatarsalgia caused by the common digital nerve becoming trapped in the metatarsal canal; the continued trauma leads to a perineural
inflammatory process that provokes endoperineural connective proliferation and hyaline degeneration of the endoneurium. This pathological entity is more commonly known as Morton’s neuroma. The term "neuroma" for the tumour found between the metatarsal heads is misleading. The lesion consists of perineural fibrosis, local vascular proliferation, oedema of the endoneurium and axonal degeneration. Macroscopically it has a typically fusiform configuration, a glistening and white appearance and a soft consistency. Histologically, this condition is characterised by fibrous degeneration of the soft tissues around the nerve and demyelination and endoneurial fibrosis of the nerve.
Most of the patients are middle-aged females. Typically, only one foot is affected and most frequently Morton’s neuroma occurs in the third interspace. The clinical signs and symptoms are characteristic; the most common symptom is a localised burning pain with tingling and numbness. Crisis of pain are triggered by walking in shoes, which most put pressure on the forefoot. During the fit patients have the urge to take off their shoe and massage their forefoot in order to provide immediate relief. Neurological signs (hypoaesthesia of the fingers involved or hyperalgesia on the tips of the fingers) are less specific.
Mulder’s manoeuvre is important in the diagnosis of the neuroma and consists of lateral compression of the metatarsal heads in alternation with plantar pressure, which tends to induce plantar dislocation of the intermetatarsal mass provoking a clicking sensation (Mulder’s click).
Instrumental examination includes radiographs in the common projections (AP, LL, weightbearing, oblique), which are intended to exclude associated pathologies.
US is the initial modality for assessing the forefoot of the patient with neuralgic metatarsalgia. Dynamic assessment with lateral compression of the metatarsal heads increases US sensitivity, allowing recognition of the neuroma as it is expelled from the intermetatarsal canal, which it entered due to plantar pressure or attraction by near structures such as the intermetatarsal bursa (which at surgery is often indistinguishable from the nerve).
MRI examination is useful when other conditions need to be ruled out (such as stress fractures, bursitis or synovitis) or to better characterise a synovial ganglion or a giant cell tumour of the tendon sheath.
There are various conservative and surgical methods of treatment: conservative methods include footwear modifications, local anaesthesia and corticosteroid injections.
For the initial stages, when there is no actual nodular enlargement of the nerve, the surgical treatment involves the simple endoscopic decompression of the TILM (transverse intermetatarsal ligament).
Dorsal neurectomy remains the effective treatment; it is performed placing the patient in a supine position under spinal anaesthesia and it consists in a 3 cm long longitudinal incision over the affected metatarsal space through the transverse intermetatarsal ligament. After sectioning this structure, and performing a slight plantar pressure, the IDN (interdigital neuroma) is identified and resected.
Morton's neuroma.




Based on the provided ultrasound and MRI images, a localized “mass-like” appearance can be observed between the heads of the third and fourth metatarsals. The main imaging features include:
1. Ultrasound: A hypoechoic or isoechoic area is detected between the third and fourth metatarsal heads, appearing elliptical in shape. During lateral compression (Mulder’s maneuver), this region may undergo dynamic deformation or be squeezed out in the intermetatarsal space.
2. MRI: In the intermetatarsal space between the third and fourth metatarsals on routine sequences (including T1, T2, and fat-suppressed sequences), a focal signal abnormality is seen: it may present as a mild or moderately low signal on T1 and as slightly high or mixed signal on T2 or fat-suppressed images (in some cases, it can appear low or moderate signal), contrasting distinctly with the surrounding fat signal.
3. No obvious bony abnormality: Routine X-ray examinations are negative, ruling out prominent fractures or significant bone lesions.
Overall, the imaging findings are consistent with thickening or fibrosis of the intermetatarsal nerve and surrounding soft tissues, sometimes accompanied by small amounts of cystic fluid or signs of bursitis in the vicinity.
Considering the clinical symptoms (local forefoot pain, no history of trauma, pain triggered by walking) and imaging findings, the following diagnoses should be considered:
Considering the patient’s age (30 years old, male), clinical presentation (forefoot pain without trauma, significant pain induced by Mulder’s maneuver), and typical ultrasound and MRI findings, the most likely diagnosis is:
Morton’s neuroma
If diagnostic uncertainty remains or if the exact neuropathological nature needs further clarification, high-resolution ultrasound examination or surgical exploration may be considered.
Rehabilitation Goal: Alleviate intermetatarsal pain, improve foot function and walking capacity, and reduce recurrence risk.
Throughout the rehabilitation process, pain symptoms and foot load should be continuously monitored. If pain recurs or any obvious abnormality emerges, seek medical advice promptly or adjust the rehabilitation program.
Disclaimer: This report is a reference analysis based on existing data. It does not replace an in-person consultation or the opinion of a qualified physician. For specific diagnosis and treatment, please follow the guidance of your primary physician.
Morton's neuroma.