Pigmented villonodular synovitis of the knee



Clinical History
A 59-year-old female patient presented with a 6-month history of spontaneous knee swelling and intermittent pain. Joint effusion was haemorrhagic on aspiration. She had no history of a bleeding disease or trauma. Physical examination revealed mechanical blockage of the knee joint.
Imaging Findings
Plain radiographs demonstrated suprapatellar swelling and degenerative changes of the knee joint (Fig. 1a, 1b).
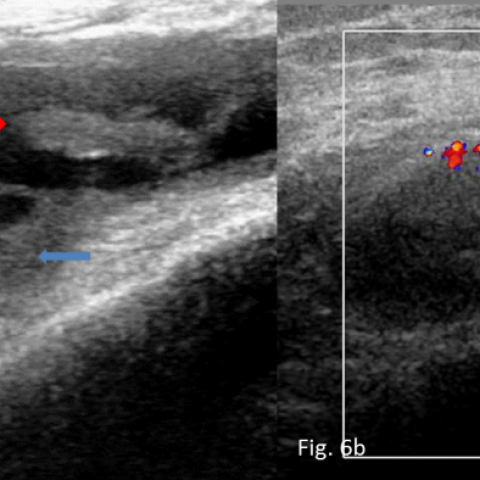
Sagittal T2-WI (Fig. 2a, 2b, 2c) and axial PD fat suppressed (Fig. 3a, 3b) MRI images disclosed joint effusion in multiple recesses demonstrating low-signal-intensity rim with nodular thickening, attributed to a thickened synovium. In T2* sequence the nodular thickened synovium presented blooming artefact consistent with deposition of haemosiderin (Fig. 4a, 4b, 4c). Sagittal T1-WI fat-suppressed postcontrast images showed enhancing synovium and villonodular synovial fronds (Fig.5a, 5b). Ultrasonography also demonstrated the joint effusion with hypertrophied synovial fronds, mildly hypervascular in colour Doppler ultrasound (Fig. 6a, 6b).
Imaging findings were consistent with diffuse pigmented villonodular synovitis, confirmed histologically after arthroscopic synovectomy (Fig. 7a, 7b).
Discussion
Pigmented villonodular synovitis (PVNS) represents an uncommon benign neoplastic process that may affect the synovial tissue intraarticularly (diffusely or focally, PVNS) or extraarticularly involving the bursa (pigmented villonodular bursitis, PVNB) or the tendon sheath (pigmented villonodular tenosynovitis, PVNTS) [1, 2]. Hypertrophic synovium may appear villous, nodular, or villonodular with prominent haemosiderin deposition. PVNS and PVNB are usually located in the knee, followed by the hip, whereas PVNTS in the hand and foot [3, 4].
Localised disease represents 77% of cases compared with 23% of the diffuse form and is frequently located in Hoffa’s fat body [5]. It usually occurs between 20-45 years of age [6]. Most of the patients present with monoarticular complaints of a soft-tissue mass, pain or swelling [5].
In PVNS of the knee, plain radiographs may appear normal or demonstrate a periarticular soft tissue density, expansion of the suprapatellar pouch and local osseous changes [8], like extrinsic bone erosions, osteopenia, joint space narrowing, intraarticular osteochondral bodies and degenerative disease, however, more frequently encountered in smaller capacity joints such as the hip, shoulder, elbow and ankle. In the hip, concentric erosion of the femoral head produces a characteristic “apple core” deformity [10]. In the diffuse form ultrasonography may reveal joint effusion, heterogeneous echogenic masses, and thickened hypoechoic synovium that may have nodular and villous projections. In the localised form a solitary focal synovial mass may be seen. Doppler imaging may detect increased blood flow [3, 7].
MRI reveals joint effusion generally surrounded by, plaque-like and less frequently villous or villonodular, thickened synovial rinds of haemosiderin-laden tissue. Synovial thickening may show intermediate-low signal intensity on T1-WI and low on T2-WI MR-images, due to T2-relaxation time shortening caused by haemosiderin. An enlargement of the low-signal-intensity areas (“blooming”), on gradient-echo-images, is consistent with the presence of haemosiderin and is nearly pathognomonic of PVNS. Variable degree of enhancement is present in post-contrast-images [9].
Additional MRI findings include bone erosion, subchondral cysts, septations, oedema in adjacent bone or soft tissue and articular cartilaginous defects [4]. MRI defines disease extent in order to guide complete surgical excision (the treatment of choice). Differential diagnosis should include a) haemophilic arthropathy, clinical history of haemophilia is necessary, b) haemorrhagic synovitis, requires history of trauma, c) rheumatoid arthritis, a systemic inflammatory disorder usually presented as a polyarticular disease, d) hypertrophic synovitis, thickened synovium does not present blooming artifact in gradient-echo-images, e) synovial haemangioma, serpentine vascular channels are invariably present [3].
Differential Diagnosis List
Final Diagnosis
Pigmented villonodular synovitis of the knee
Liscense
Figures
Plain film

MR

MR

MR

MR

Ultrasound
Musculoskeletal joint

Medical Imaging Analysis Report
I. Radiographic Findings
Based on the X-ray and plain MRI images provided by the patient, soft tissue swelling can be observed in the right knee joint cavity, along with a noticeable joint effusion signal in the joint space. The synovium is thickened, showing nodular or villous proliferations in certain areas. On MRI, the T1-weighted images display moderate or slightly low signal intensity, while the T2-weighted images exhibit significantly reduced signal. A “blooming” effect can be seen on the gradient echo sequence, suggesting hemosiderin deposition. Some images show mild edema or inflammatory changes in the soft tissue around the joint. Slight bone erosion is noted along the articular margins, but there is no obvious new bone formation or noticeable fracture line.
In summary, the imaging reveals diffuse or focal synovial thickening in the knee joint, primarily presenting as low signal, with characteristic “blooming” effects due to hemosiderin deposition. Additionally, minor bone erosion near the articular surface is consistent with pressure or invasion of the bone surface by synovial lesions.
II. Potential Diagnoses
- Pigmented Villonodular Synovitis (PVNS): The typical finding is synovial thickening in or around the joint, with low signal intensity and “blooming” effects caused by hemosiderin deposition, often accompanied by joint effusion and bone erosion.
- Hemorrhagic Synovitis: If there is a history of trauma or coagulopathy, repeated joint bleeding may lead to synovial changes. However, the patient has no significant history of trauma or bleeding disorder, making this less likely.
- Rheumatoid Arthritis: Commonly presents with multiple joint involvement and synovial thickening. The “blooming” sign due to hemosiderin is not typical, and it is often associated with elevated systemic inflammatory markers.
- Hypertrophic Synovitis (Other Non-specific Inflammatory Causes): Synovial thickening can be diffuse, but the “blooming” sign on gradient echo sequences is usually not pronounced.
- Synovial Hemangioma: Imaging may show characteristic “flow voids” or curvilinear vascular signals, and the clinical history could include recurrent spontaneous bleeding. However, its imaging features differ from those in this case.
III. Final Diagnosis
Considering the patient’s age (59 years), clinical manifestations (spontaneous swelling of the knee joint, intermittent pain, and mechanical locking symptoms), blood-tinged joint effusion without a history of bleeding disorders or trauma, and the low-signal synovium with significant hemosiderin “blooming” on MRI, the most likely diagnosis is:
Pigmented Villonodular Synovitis (PVNS).
For further diagnostic confirmation, arthroscopic synovial biopsy can be performed to verify the typical pathological features of “hemosiderin deposition, villous synovial proliferation, and giant cells.”
IV. Treatment Plan and Rehabilitation Program
1. Treatment Strategy
- Arthroscopic or Open Synovectomy: For localized or diffuse PVNS, a complete synovial resection should be performed whenever possible to reduce recurrence.
- Adjuvant Therapy: In cases of diffuse disease or high risk of postoperative recurrence, adjuvant radiotherapy may be considered after surgery, but should be used with caution.
- Joint Stability and Functional Rehabilitation: Postoperative rehabilitation exercises are essential to restore range of motion and strengthen the surrounding musculature as early as possible.
2. Rehabilitation/Exercise Prescription Recommendations (FITT-VP Principle)
After confirming proper wound healing and joint stability post-surgery, a gradual, individualized rehabilitation plan is recommended:
- Frequency (F): Conduct rehabilitation training 3-5 times per week. In the early postoperative phase, starting with 3 sessions per week is advisable.
- Intensity (I): Begin with low-intensity joint mobility exercises (passive or assisted active knee movements). As pain decreases and joint stability improves, gradually incorporate muscle-strengthening exercises (e.g., resistance band exercises, light weight-bearing).
- Time (T): Each session can begin at 15-20 minutes, gradually increasing to 30 minutes or more as tolerance improves.
- Type (T): Utilize aquatic therapy (to reduce joint load), static and dynamic muscle strengthening (e.g., isometric quadriceps contractions), and active knee flexion/extension exercises. Later, introduce mild resistance training and other modalities.
- Progression (P): Adjust the plan according to pain levels, range of motion, and swelling. If the joint is stable, gradually add balance, posture control, and lower limb endurance training (e.g., stationary cycling or elliptical).
- Volume and Personalization (VP): Adjust training intensity and volume based on body weight, knee function scores, cardiopulmonary fitness, and bone condition. Progress gradually according to individual needs.
Safety Note: Because the patient is nearly 60 years old, close attention should be paid to cardiovascular function and bone health. If significant pain or swelling recurs, training should be paused or modified, and follow-up examinations should be conducted.
Disclaimer
This report is based solely on the provided imaging and medical history, serving as a reference for clinical diagnosis and treatment. It does not replace in-person consultation or professional medical advice. If you have any questions or experience any changes in your condition, please seek prompt medical attention or consult a specialist.
Human Doctor Final Diagnosis
Pigmented villonodular synovitis of the knee