A case of myositis ossificans traumatica



Clinical History
A 6-year-old male patient with a history of trauma and left thigh pain.
Imaging Findings
A 6-year-old child arrived at our department after a left thigh trauma (falling on stairs).
Femur RX was performed, showing no fractures (Fig. 1).
Pain did not cease and functional limitation persisted, so after 20 days the patient repeated left thigh radiography:
Near femur diaphysis RX shows calcifications in the quadriceps muscle bellies (Fig. 2).
US confirmed these finds.
Then MR was performed showing a lesion at vastus intermedius of left quadriceps (11x3.5x1.5 cm). This lesion presented signal inhomogeneity with hypointense areas corresponding to calcifications and inhomogeneous enhancement after contrast injection (Fig. 3).
Patient was treated with rest and US, two months later another MR was performed, showing reduction of the lesion and the perilesional oedema (Fig. 4).
Currently the child has no pain and no functional impairment.
Discussion
Myositis ossificans traumatica (MOT) is often defined as heterotopic, non-neoplastic proliferation of bone in an area previously exposed to trauma and haematoma.
The most common areas that are affected by MOT are the quadriceps femoris, brachialis anticus, and the adductor muscles of the thigh although it may occur anywhere. It can happen at any age, but occurs most frequently in adolescents and young athletes, with over half of the cases occurring in the third decade. MOT is considered rare in children under 10 years of age and males are more often affected than females [1-2].
The pathogenesis of this injury remains unclear at this time. Some of the common theories include:
transformation of muscle haematoma to bone;
haematoma calcification;
intramuscular bone formation from detached periosteal flaps;
osteoblast proliferation from periosteal rupture;
metaplasia of intramuscular connective tissue cells;
individual predisposition.
It is believed that blunt trauma to the extremity creates a compression wave travelling through soft-tissue crushing the deepest muscle against the bone. The force is transmitted through the fluid compartment of all of the layers of muscles but the damage usually occurs in the layer that is next to the bone.
A typical patient presentation includes a history of trauma to the affected area with increased difficulty in moving and using the affected limb. The onset seems to be related to the severity of the injury. Pain, swelling and tenderness of the affected area usually do not respond to conservative management within the first 4–5 days.
Active, passive and resisted range of motion will be notably decreased in the affected limb with more severe injuries [2-3].
Three important criteria are to consider when diagnosing MOT. These include:
a history of significant local injury;
clinical and radiological evidence of ossification within 2 months of the initial injury;
the location of the lesion in proximal limb areas more commonly associated with MOT including the brachialis anticus and quadriceps femoris [3].
MOT is generally considered to be a self-limiting condition and can have spontaneous resolution. Without treatment the radiological and clinical findings stabilise and/or resolve within 1.5 to 3 years following the onset of symptoms. Full reabsorption can take place especially in lesions occurring within the muscle belly. Lesions located near an origin or insertion of a muscle are less likely to reabsorb and may result in functional impairment.
Differential Diagnosis List
Final Diagnosis
Myositis Ossificans Traumatica (MOT).
Liscense
Figures
Femur RX


Femur RX 20 days after


Thigh MRI



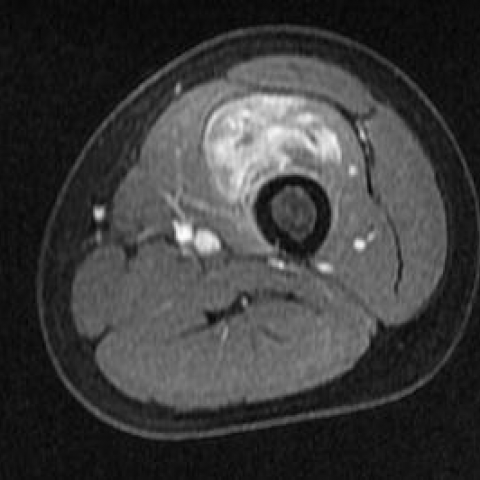
Thigh MRI after two months


Imaging Findings
Based on the provided X-ray and MRI images of the left thigh, there are localized abnormal densities or signal changes in the surrounding soft tissues near the femur:
- On the X-ray, irregular calcifications within the local soft tissue are observed, appearing in relatively layered or ring-shaped distributions. No significant cortical bone destruction or notable periosteal reaction is seen.
- The MRI shows that the lesion is confined to the muscle layer, displaying a mixed high- and low-intensity signal around the lesion. There is noticeable soft tissue swelling and a T2 hyperintense signal in the affected area. A dark signal ring suggesting calcification or ossification may be present around the periphery or boundary of the lesion.
- No obvious fracture lines or destructive changes of the femur are observed. There is no significant evidence of tumoral infiltration or bone marrow involvement in the surrounding tissues.
Possible Diagnoses
Considering the patient's history of trauma and imaging findings, the following diagnoses are possible:
- Myositis Ossificans Traumatica (MOT)
Reason: This commonly occurs as ossification or calcification within soft tissue after trauma. It frequently appears in young adults or individuals with a clear history of injury. On X-ray and MRI, newly formed bone or calcification can be found within the soft tissue where no bony structure previously existed. The history of trauma and the gradual appearance of calcifications are consistent with this diagnosis. - Soft Tissue Sarcoma (e.g., osteosarcoma with soft tissue components or other soft tissue tumors)
Reason: A tumor may also present with soft tissue swelling and calcification. However, the calcification pattern is typically irregular and often accompanied by more aggressive behavior or bone destruction. The patient’s age and clinical course may not fully match such a scenario. - Others: Infection or Traumatic Pseudotumor
Reason: Infectious calcification or inflammatory soft tissue lesions can also present with abnormal signals or densities. However, these are usually accompanied by acute inflammatory signs (e.g., redness, swelling, heat, pain, abnormal lab results) and may exhibit other local or systemic signs of infection.
Final Diagnosis
Taking into account the patient’s age (6 years old), clear history of trauma, clinical symptoms (pain and discomfort in movement after injury), and the localized soft tissue ossification/calcification shown on imaging, the most likely diagnosis is:
Myositis Ossificans Traumatica (MOT).
This condition typically leads to notable soft tissue calcification or ossification about 1–2 months after trauma. The lesion often develops in the deeper muscular bundles near the adjoining bone in the muscle belly. The imaging features often show a more lucent center with relatively denser peripheral layers (zonal pattern of calcification), consistent with the findings in this child. If subsequent clinical and imaging follow-up reveals stabilization or resorption of the lesion, it would further confirm the diagnosis.
Treatment and Rehabilitation Plan
Myositis Ossificans Traumatica is generally self-limiting in most cases, with gradual improvement or stabilization. For this case, the following measures and rehabilitation plan may be considered:
- Conservative Treatment:
- Acute phase (within a few days to 2 weeks post-injury): Local immobilization and protective rest, avoid further impact or excessive stretching. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used under medical guidance according to the level of pain. Local physical therapy (such as warm compresses) can help relieve pain and improve blood circulation.
- Subacute – Recovery phase: After symptoms improve, gradually increase the range of motion. Begin gentle joint mobility and stretching exercises, avoiding overly forceful stretching of the injured muscles.
- Surgical Treatment
If the lesion continues to enlarge, pain becomes unmanageable, or it significantly interferes with joint function, and if the lesion remains stable 6–12 months after injury but still notably impacts daily activities, surgical excision may be considered after evaluation by a physician. However, surgery is usually deferred until the lesion is mature to reduce the risk of recurrence. - Rehabilitation/Exercise Prescription Advice (FITT-VP Principle):
- Frequency: It is recommended to have professional rehabilitation sessions 2–3 times a week, accompanied by low-intensity activities on other days to prevent muscle atrophy.
- Intensity: Initially, use low-load, low-resistance exercises (such as eccentric training or core stability work). Employ gentle stretching and isometric contractions within the tolerable range of pain.
- Time: Start with about 10–15 minutes per session, then progressively increase to around 30 minutes, adjusting according to the patient’s tolerance.
- Type: Prioritize exercises that do not impose excessive impact on the affected area, such as straight-leg raises in proper alignment, short walks, support exercises, and low-load machine-based training.
- Volume and Progression: As pain subsides and joint range of motion improves, gradually increase exercise intensity and duration. Avoid overexertion or reinjury.
If the child has any other comorbidities or skeletal development abnormalities, exercise intensity and methods should be adjusted under specialist guidance, taking into consideration bone growth characteristics to avoid adversely affecting long bone development or joint function.
Disclaimer: This report is a reference-based medical analysis based on currently available imaging and clinical history, and it does not replace an in-person consultation or the professional advice of a physician. If problems persist or symptoms worsen, please consult a doctor and undergo relevant examinations promptly.
Human Doctor Final Diagnosis
Myositis Ossificans Traumatica (MOT).