

10-year-old boy with bilateral knee pain for one year, swelling after activity and morning stiffness. No history of trauma, locking or giving way.
On examination normal gait but flexion over 90 degree was uncomfortable, X-ray showed some irregularity of distal femoral articular surface.
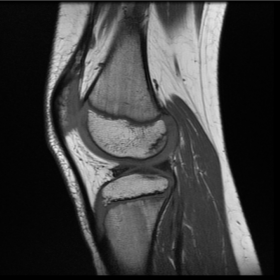
Appearances are identical in both right and left knee with irregularity of the posterior aspect of both medial and lateral femoral condyles with thickened overlying articular cartilage. Normal medial and lateral menisci. There is irregularity of posterior aspect of both medial and lateral femoral condyles and more marked laterally. The overlying articular cartilage is thickened. No marrow oedema. No joint effusion. Normal ACL PCL, MCL and lateral collateral complex. Normal patellar articular cartilage and the articular cartilage in the trochlea groove.
Discussion Ossification variability of the femoral condyle mimics osteochondritis dissecans (OCD), With the increasing reliance on MR for the evaluation of knee disease in children, an understanding of the normal MRI appearance of the developing femoral condyle is important to differentiate this from disease. The developmental sequence of OCD begins with the separation of the subchondral bone. Trauma or repetitive microtrauma in a rapidly growing individual may compromise the blood supply by the epiphyseal artery, resulting in an osteochondral lesion [1]. Juvenile OCD is twice as common in male as in female patients and is more frequent in athletically active children .Poorly localised knee pain, stiffness and swelling are typical symptoms. Mechanical symptoms like grinding and locking are associated with the late stages of OCD where loose osteochondral lesions are present [1].
The classic location of OCD is on the lateral aspect of the medial femoral condyle. High prevalence of subchondral bone defects of the ossifying femoral condyle on MRI makes it difficult to diagnose weather this is a normal variant of ossification or OCD. Gebarski et al. stated that defects in the posterior femoral condyles with intact cartilage, accessory ossification centres, spiculation, greater physeal cartilage and lack of BME are features of ossification variability[2]. Lennart B. O. Jans described that a lesion angle <105° was a feature of ossification variability. Ossification variability does not occur when there is less than 20% residual physeal cartilage of the femoral condyle, OCD is rare with residual physeal cartilage greater than 20%. Location in the intercondylar part of the femoral condyle is seen in OCD only [3].
It is important to differentiate OCD, requiring conservative and/or surgical treatment, from ossification variability [4]. OCD has been classified in the literature as stable or unstable by MRI criteria [1]. Stable lesions are amenable to conservative treatment, including activity modification and knee immobilisation. Failure to demonstrate healing on MRI after 6–12 months is considered failure of conservative management [5]. Failed conservative management or unstable lesion requires surgical intervention. In our case we came to the conclusion that MRI finding were a normal variant of ossification. Patient was reviewed in clinic 3 months later and his knee symptoms improved, the patient was doing well and was hence discharged. On MRI interpretation the above written explanation will help in differentiating the ossification variability from OCD.
Normal ossification variability of femoral condyle




Based on the provided knee joint MRI images and the patient’s clinical presentation (bilateral knee pain, swelling after activity, and morning stiffness), the following imaging characteristics can be observed:
Based on the imaging characteristics above and the patient’s medical history, the possible diagnoses or differential diagnoses include:
Taking into account the patient’s age, bilateral knee symptoms persisting for one year without a significant history of trauma or joint locking, the MRI findings showing no marked subchondral edema or destructive changes, and the gradual alleviation of symptoms upon follow-up, these irregular areas are more likely normal ossification variations. Therefore, the most likely final diagnosis is: epiphyseal developmental variability (normal variation), which does not match the classic signs of Osteochondritis Dissecans (OCD).
Given that the patient’s symptoms are not progressively worsening and that the MRI findings suggest a normal variation in epiphyseal development, treatment should primarily focus on conservative observation and functional exercises:
Disclaimer: This report is provided solely as a preliminary analysis of the imaging and clinical information and does not replace a formal in-person consultation or professional medical advice. Please follow the final evaluation and recommendations of a specialist physician for an exact diagnosis and treatment plan.
Normal ossification variability of femoral condyle