Extensive regional non infective myonecrosis following a transfusion extravasation


Clinical History
40-year-old female patient with acute regional forearm pain and flexor compartment swelling following the second unit of a blood transfusion (transfusion was immediately stopped). An emergency fasciotomy was then performed. While the swelling resolved, the patient continued to lose function corresponding to all flexor and some extensor arm muscles.
Imaging Findings
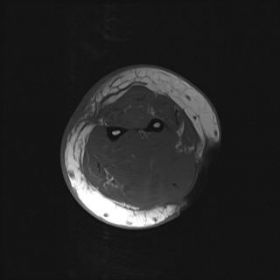
Axial T1 weighted image shows (Fig. 1) evidence of a fasciotomy and loss of fat planes but no appreciable intrinsic muscle abnormality while the T2 weighted fat saturated image (Fig. 2) shows widespread oedema represented by extensive high signal involving almost all of the flexor compartmental muscles as well as some of the muscles in the extensor compartment and surrounding soft tissues. On T1 post contrast fat suppressed images (Fig. 3, 4), there is widespread non enhancement involving almost all of the flexor compartment musculature and well as some of the extensor compartment musculature. Flow void as well as contrast enhancement is observed within the surrounding subcutaneous veins indicating satisfactory venous drainage (Fig. 4) and therefore implying some intact arterial supply. There were no clinical or biochemical features to suggest any infection making intramuscular abscesses unlikely. Therefore a regional non-infective myonecrosis was considered the most likely diagnosis.
Discussion
Myonecrosis is a term referring to death of muscle and can occur in a number of situations. On MRI, it is characterised by non enhancement of muscle. Perifascial fluid collections, subcutaneous oedema, peripheral enhancement of muscle following contrast have also been described as adjunctive MRI findings [1].
Among the many causes of myonecrosis include diabetic myonecrosis [2, 3, 5], chronic graft versus host disease (GVHD) [3], various drug overdoses (e.g. heroin, cocaine, barbiturates [4]), sickle cell crises, crush injuries, severe ischaemia, intra-arterial chemotherapy and various conditions causing rhabdomyolysis.
Focal (or regional) myonecrosis has been described following compartmental syndrome but usually occurs before a fasciotomy or when a fasciotomy has been delayed [3].
An unusual feature in this case is that the myonecrosis extends beyond one compartment (i.e. involves both the flexor and extensor compartments) which implies that a pure compartment syndrome could not have been the sole causative factor.
Rhambdomyolysis has previously been reported to occur with heparin [3] which may have been a possible contributor in this case especially considering the patient receiving a blood transfusion immediately prior to the event, although this is not proven in this case.
Differential Diagnosis List
Final Diagnosis
Regional myonecrosis
Liscense
Figures
MR

MR

MR

MR

1. Imaging Findings
Based on the provided MRI images, the following main features are observed:
- In the cross-sectional view of the forearm, part of the muscle tissue exhibits significant signal abnormalities. On T1-weighted images, the muscle signal is decreased or mixed, indicating damage to muscle fiber structures.
- On T2 or other fluid-sensitive sequences (e.g., STIR), the affected muscle area shows increased signal, with evidence of peripheral tissue edema or fluid accumulation.
- After contrast enhancement, there is extensive uneven or absent enhancement in the muscles, suggesting possible necrotic or ischemic zones in the muscle fibers. Ring-shaped or irregular enhancement may be seen around the muscle and fascia.
- Edema or fluid is not confined to a single compartment in the forearm; it also involves part of the extensor compartments, covering a relatively wide range.
These findings correlate with the patient’s postoperative clinical condition (emergency fasciotomy for compartment decompression): although acute swelling has subsided, muscle function is still impaired, and there is concern for a significant degree of muscle necrosis.
2. Possible Diagnoses
Taking into account the patient’s history (acute forearm swelling, interrupted blood transfusion, urgent fasciotomy for decompression) and the imaging findings, the following considerations arise:
- Acute Myonecrosis:
In this case, the MRI shows widespread absence of enhancement and abnormal signals in the muscles, suggesting muscle fiber necrosis. The injury may be secondary to multiple causes, such as severe local ischemia, rhabdomyolysis, or compartment syndrome. Based on the clinical picture, myonecrosis is the primary consideration.
- Incomplete Relief or Complication of Compartment Syndrome:
Although an emergency fasciotomy has been performed, if the surgical decompression was insufficient or the tissues were compressed for too long, irreversible muscle fiber necrosis may still occur. The current imaging suggests the necrosis extends beyond a single muscle compartment, indicating more extensive involvement.
- Rhabdomyolysis:
The use of certain medications (e.g., heparin) or other factors (including metabolic disorders, transfusion-related complications, or ischemia-reperfusion injuries) may trigger rhabdomyolysis, resulting in localized muscle necrosis and functional impairment. On MRI, the necrotic areas may also present local or diffuse abnormal muscle signals.
3. Final Diagnosis
Considering the patient’s age, the acute onset, clinical history (blood product transfusion, sudden local swelling, fasciotomy for decompression), and MRI findings showing obvious muscle necrosis with heterogeneous enhancement over a wide range, the most likely diagnosis is:
“Acute Myonecrosis”
The imaging results and clinical course indicate that the necrosis is not limited to a single compartment but also involves part of the extensor compartment, consistent with severe or multifactorial causes. This case may involve compartment syndrome combined with other contributing factors (e.g., rhabdomyolysis, adverse reactions to blood products or medications).
4. Treatment and Rehabilitation Plan
- Treatment Strategy:
- Continue closely monitoring local tissue perfusion and the extent of muscle necrosis. Repeat MRI or ultrasound may be required to assess blood flow.
- Following fasciotomy, if residual high pressure or incomplete decompression persists, further exploration or enlargement of the decompression area may be needed.
- To address infection risk, absorption of necrotic muscle tissue, and prevention of complications, antibiotics (if infection is suspected) and debridement of necrotic tissue may be necessary.
- Monitor muscle enzyme levels (e.g., CK), renal function, and electrolyte changes to anticipate or manage complications of rhabdomyolysis (such as acute kidney injury).
- If there is a clear medication-related factor (e.g., adverse reaction to heparin), discontinue or switch the offending drug and initiate supportive care.
- Rehabilitation and Exercise Prescription (FITT-VP Principle):
After the acute inflammatory or necrotic phase, initiate functional rehabilitation and physical therapy promptly, with gradual progression and individualization:
- Initial Phase (Acute/Early Postoperative) - Light Intensity:
- Frequency (F): 1–2 times per day with simple passive joint movements, avoiding secondary injury.
- Intensity (I): Should not cause marked pain or exacerbate edema. Initially, a therapist can assist with gentle joint mobilization.
- Time (T): 5–10 minutes per session, gradually increasing.
- Type (T): Passive joint movements, gentle muscle activation (e.g., making a fist, wrist movement).
- Progression (P): As pain and swelling become tolerable, gradually increase the range of motion and frequency.
- Middle Phase (Functional Restoration):
- Frequency: 3–5 sessions per week.
- Intensity: Low-load resistance training (e.g., resistance bands) to maintain or gradually restore muscle strength.
- Time: 15–20 minutes or more per session, adjusted as tolerated.
- Type: Safe-range active joint movements, isometric or low-intensity isotonic exercises, possibly combined with aquatic therapy or partial weight-bearing exercises.
- Progression: Increase resistance and range of motion cautiously, avoiding excessive stretching or fatigue.
- Late Phase (Strength and Coordination Recovery):
- Frequency: 3–4 times per week.
- Intensity: Progressively moderate; may incorporate light weight training (e.g., dumbbells, light barbells).
- Time: About 30 minutes per session, depending on tolerance.
- Type: Exercises to enhance joint flexibility and muscle balance, combined with functional training (e.g., median or ulnar nerve mobilization) to prevent adhesions.
- Progression: Increase variety and load in the absence of significant pain, swelling, or inflammation.
Throughout the rehabilitation process, regularly evaluate postsurgical recovery as well as neurovascular function. Discontinue and re-evaluate if severe pain or localized swelling occurs again.
- Initial Phase (Acute/Early Postoperative) - Light Intensity:
Disclaimer: This report is a reference analysis based on the current patient history and imaging data provided. It does not replace in-person evaluation or professional medical advice. If there are additional clinical concerns or changes in symptoms, prompt medical consultation or further specialized examinations are recommended.
Human Doctor Final Diagnosis
Regional myonecrosis