Imaging findings in Morel-Lavallée lesion



Clinical History
30-year-old male patient with history of trauma to the right knee and lower thigh 2 weeks earlier during a soccer match. The patient complained of a swelling over the medial aspect of the right lower thigh which was progressively increasing in size.
Imaging Findings
Ultrasonography showed a well defined oval hypoechoic lesion with internal septations in the medial aspect of lower thigh with no evidence of internal vascularity entirely limited to the subcutaneous plane.
CT showed a hypodense fluid attenuation lesion in the subcutaneous plane of the lower thigh in the medial aspect causing minimal compression on the vastus medialis muscle.
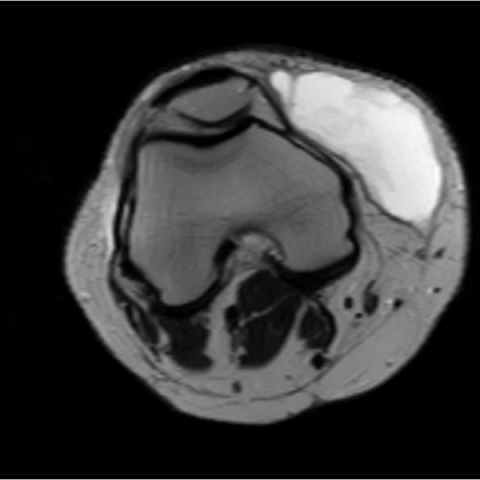
MRI showed a well defined lesion in the medial aspect of the lower thigh limited to the subcutaneous perifascial plane (between subcutaneous fat and deep fascia). The lesion appeared heterogeneously hyperintense on T2W and STIR sequences and predominantly hyperintense on T1W images (suggestive of subacute hemorrhage). Internal septations and fluid-fluid levels were noted. Focal internal areas of T1 hyperintensity were noted showing suppression on STIR images- suggestive of areas of fat necrosis.
Incision and drainage confirmed the presence of altered blood within the lesion.
Imaging and operative findings were diagnostic of Morel-Lavallée lesion.
Discussion
Morel-Lavallée lesions are soft tissue injuries characterised by post traumatic fluid collections dissecting subcutaneous fatty tissue. The pathogenesis of the lesion consists of shearing or tangential forces causing separation of skin and subcutaneous tissue from the underlying fascia [1, 2, 3].The injury causes disruption of perforating vessels and creation of a potential space which gets filled with blood , lymph, debris and fat (secondary to fat necrosis) [3]. Various names have been attributed to Morel-Lavallée lesions in literature such as posttraumatic soft-tissue cysts, pseudocysts, Morel-Lavallée extravasations or Morel-Lavallée effusions [1, 2, 4]. Although initially described in the trochanteric and proximal thigh region, these lesions may also involve the abdominal wall, buttock, lower thigh and scapular region [1, 2, 5].
Imaging findings confirm the location of the lesion in the subcutaneous perifascial plane. On ultrasonography, Morel-Lavallée lesions appear hypoechoic with internal septations. CT images may demonstrate fluid/blood attenuation. On MRI, the lesions show variable signal intensity. Important diagnostic clues include fluid-fluid levels, internal septations and focal areas of fat within the lesion. The finding of internal fat is an important diagnostic tool which radiologists should actively seek [5]. The lesions may have no demonstrable capsule, a partial capsule or complete capsule which if present appears hypointense on all pulse sequences due to fibrosis or haemorrhagic byproducts [6]. Mallado et al proposed a useful MRI classification system of Morel-Lavallée lesions including six subtypes [7].
Type I: Laminar shaped, seroma-like with decreased T1 and increased T2 signal.
Type II: Oval shaped with increased T1 and T2 signal (subacute haematoma).
Type III: Oval shaped with intermediate T1 and heterogeneous T2 signal (chronic organising haematoma), thick capsule and internal/peripheral enhancement.
Type IV: Linear shaped like a closed laceration with hypointense T1 and hyperintense T2 signal.
Type V: Pseudonodular (round shape) with variable T1/T2 signal and internal/peripheral enhancement.
Type VI: Infected with variable T1 and T2 signal, sinus tract formation, thick capsule and internal/peripheral enhancement.
Prepatellar bursitis can mimic a Morel-Lavallée lesion when it occurs near the knee joint. The size of the bursal collection is usually smaller when compared to Morel-Lavallée lesions. Prepatellar bursal collections also do not cross the midcoronal plane to extend into the posterior aspect of the knee joint [5].
Chronic lesions may lead to a misdiagnosis of soft tissue tumour owing to irregular enhancement [4].
In acute settings, surgery is recommended. Other modes of treatment include compression and doxycycline sclerodesis [7, 8].
Differential Diagnosis List
Final Diagnosis
Morel-Lavallée lesion
Liscense
Figures
Ultrasound



CT


MRI






1. Imaging Findings
Based on ultrasound, CT, and MRI imaging findings, this patient presents a conspicuous fluid-density/signal region in the subcutaneous fascial plane of the right knee joint and the proximal medial thigh, with a relatively well-defined shape and clear contour. On ultrasound, the lesion appears as a hypoechoic area with internal septations. On CT, it is seen as a low-density lesion within the superficial fascial layer, with no evident bony destruction. On MRI, it shows low or intermediate T1 signals and high T2 signals, with more complex internal signals observed in some slices (possibly suggesting fatty components or gradually organized blood products). The lesion demonstrates a relatively clear interface with surrounding soft tissue and does not significantly involve the joint cavity or deep muscular structures.
2. Potential Diagnoses
Considering the patient’s trauma history and imaging characteristics, possible diagnoses include:
- Morel-Lavallée lesion: The primary consideration. Typically presents as a fluid or fat-containing fluid accumulation caused by the separation of the subcutaneous fat layer from the deep fascia, often associated with a history of trauma. On imaging, it commonly shows mixed signals on various sequences and a cystic structure.
- Local hematoma or tumor-like soft tissue lesion: If the separation from the fascial plane is not clear, subacute or chronic hematoma should be considered. However, its morphology, tissue plane, and clinical history are more consistent with a Morel-Lavallée lesion.
- Bursitis (e.g., prepatellar bursitis): When an adjacent knee bursa is distended with fluid, it may resemble a Morel-Lavallée lesion but is usually confined to the bursa and does not span separate fascial planes.
3. Final Diagnosis
Taking into account the patient’s youth, history of trauma (impact or shearing force from playing football), the localized subcutaneous fluid collection, the typical imaging presentation, and progressively increasing swelling, the most likely diagnosis is:
Morel-Lavallée lesion
4. Treatment Plan and Rehabilitation
Based on the features of a Morel-Lavallée lesion and clinical experience, the following treatment approaches may be considered where appropriate:
- Conservative treatment: For smaller lesions with mild symptoms, compression bandaging or compression stockings can be applied to reduce fluid accumulation and facilitate absorption, alongside regular follow-up imaging to monitor changes in the lesion.
- Aspiration/drainage or sclerotherapy: If fluid accumulation is significant, continuously enlarging, or causes functional impairment, aspiration may be performed, with chemical sclerosis (e.g., doxycycline) considered to reduce recurrence.
- Surgical intervention: For lesions that are large in size, have a well-defined capsule, or are refractory to treatment and prone to recurrence, surgical debridement and fascial repair may be conducted to prevent re-accumulation and infection.
Rehabilitation and Exercise Prescription (FITT-VP Principle):
- Training Frequency (Frequency): During the acute phase and early treatment, it is recommended to engage in low-intensity exercise 2-3 times per week. After symptoms have improved, gradually increase to 3-4 times per week.
- Training Intensity (Intensity): Start with low-intensity, low-load exercises, avoiding activities that seriously twist or impact the knee joint. Increase intensity gradually according to the patient’s tolerance and pain response.
- Training Duration (Time): Begin each session with 10-15 minutes and gradually extend to 20-30 minutes, depending on recovery progress.
- Training Type (Type): Early-stage exercises may involve passive knee joint movements, straight-leg raises, and small-range flexion and extension. Later, low-impact aerobic exercises (e.g., cycling, swimming) and quadriceps/hamstring strengthening can be introduced.
- Volume & Progression (Volume & Progression): As recovery advances, increase exercise duration and load every week or two, based on pain level and joint function assessment. If pronounced swelling or severe pain arises, reduce or suspend training and re-evaluate promptly.
Disclaimer
This report is a reference analysis based on current imaging and clinical history, and does not replace an in-person consultation or advice from a professional physician. Specific diagnoses and treatment plans should be determined by a qualified physician through a comprehensive clinical assessment.
Human Doctor Final Diagnosis
Morel-Lavallée lesion