Morquio B型综合征



临床病史
一名14岁女孩自5岁开始出现鸭步步态、膝外翻及轻度脊柱侧弯。智力正常。12岁时发现生长迟缓。进行了脊柱、骨盆和全腿的平片检查,以及髋关节的MRI检查。
影像学表现
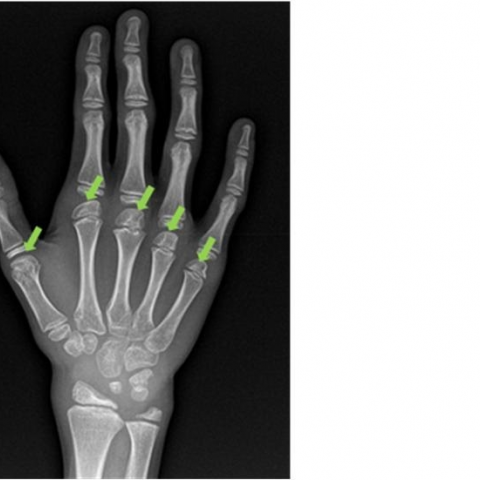
平片显示整个骨骼范围内出现弥漫性改变。最显著的发现包括齿状突发育不良、脊柱侧凸以及整个脊柱椎体扁平且呈楔形改变(图1、2)。全腿X线片显示膝外翻(图3)。手部X线片示掌骨头“方形”改变,腕骨(尤其是舟状骨)骨化延迟,以及桡尺远端骺发育不良(图4)。骨盆异常表现为明显的髋关节发育不良,股骨头扁平,髋臼浅(图5)。髋关节MRI显示股骨头严重塌陷、双侧半脱位及关节积液(图6)。生化检测提示Morquio综合征B型诊断,基因检测结果(p.Trp273Leu突变)也证实了这一诊断。
病情讨论
Morquio综合征或黏多糖贮积症 (MPS) IV型是一种由于酶缺陷导致角质硫酸盐降解缺陷的罕见遗传性疾病 [1]。存在两种非等位基因变异,分别为A型和B型。其中B型病情较轻且更为罕见 [2]。1976年,O’Brien等 [3] 首次对其进行了描述。与Morquio A型患者相比,B型不会累及中枢神经系统 [4]。由于骨和软骨中角质硫酸盐沉积,二者的骨骼表现相似,并与其他黏多糖贮积症(“多发性成骨障碍”)相似。
临床表现包括身材矮小、角膜混浊和胸廓畸形。与其他黏多糖贮积症不同的是,智力正常。
对Morquio B型患者的肌肉骨骼系统进行体格检查可发现远端关节韧带松弛、近端关节僵硬,导致鸭步样步态 [5]。典型的放射学特征包括齿突发育不良、椎体扁平、椎体呈舌状(伴有“中央尖突”)、骨骺发育不良、髋关节发育不良、髋臼浅、髂骨翼狭窄、髋内翻和膝外翻。与其他黏多糖贮积症相比,破坏性的髋关节病变通常更为严重。手部X线可显示桡骨和尺骨远端发育不良、掌骨头呈方形及腕骨小或缺失。
MRI可用于评估髋关节破坏的程度。影像学可能显示陡峭斜位的髋臼顶、股骨头扁平以及早期退行性改变 [6]。
尿液检测可能不足以确诊MPS IVB,必须进行酶学分析以评估β-半乳糖苷酶缺陷。尽管Morquio的诊断基于临床检查、生化和基因检测的综合判断,但医学影像学可以为疾病进展和并发症监测提供重要信息。最重要的是,它能够检测齿状突发育不良,这可能导致寰枢椎半脱位,最终危及生命 [7]。
虽然新的治疗手段正不断出现,但目前对Morquio综合征患者的管理主要仍以对症治疗为主,并致力于控制急性和慢性疼痛症状。康复和纠正膝外翻畸形对维持功能具有重要意义。酶替代疗法(ERT)和造血干细胞移植(HSCT)目前正在MPS IV患者中进行研究。虽然ERT和HSCT并不能治愈疾病,但它们可能会改变疾病的自然史 [8]。其他有潜力的治疗方法,例如基因治疗或小分子治疗,目前也在积极研究中。
鉴别诊断列表
最终诊断
黏多糖贮积症IVB型(莫尔基奥综合征B型)
证书
没有可翻译的英文内容。
图像分析
颈椎屈曲位侧位普通X线片

普通X线片

全腿X线片

手部普通X线片
骨盆平片

冠状面图像

影像学发现
1. 颈椎侧位片可见齿状突(齿突)发育不良,椎体呈扁平化(扁平椎)。部分椎体可见“舌状突起”或“中央楔形改变”,提示软骨内异常发育。
2. 全脊柱影像提示轻度脊柱侧弯(scoliosis),并伴有椎体变扁、椎间隙相对增宽等征象。
3. 骨盆和髋关节平片可见髂骨翼发育不良、髋臼浅,股骨头形态不规则,提示髋臼发育不良和股骨头早期退变。
4. 双下肢全长片示明显的膝内(外)翻畸形(此病例为膝外翻,即 genu valga)。
5. 手部X线可见掌骨头呈方形改变,部分远端桡尺骨发育不良,腕骨小或缺失,提示与其他黏多糖贮积症类似的“多发骨骼异常”表现。
潜在诊断
1. Morquio 综合征(MPS IV):患者存在步态蹒跚、身材矮小、髋关节发育不良、韧带松弛和其他骨骼改变,且智力正常,与MPS IVB亚型的临床特点和影像学表现相吻合。
2. 其他黏多糖贮积症(MPS 系列):部分类型也可出现多发骨骼异常(如MPS I、II、VI等),但结合患者智力正常情况及临床症状,MPS IV更符合。
3. 先天性骨骼发育不良(如软骨发育不全等):亦可出现四肢畸形、身材矮小等,但多有特异性外观与不同的颅或椎体改变,且通常与黏多糖贮积症的特异性改变可作区分。
最终诊断
基于患者自幼出现的步态异常(“鸭步”)、膝外翻、轻度脊柱侧弯,以及X线和MRI所见的齿突发育不良、髋关节破坏、骨骼发育异常等综合分析,同时患者智力正常,最符合 Morquio 综合征(MPS IV)B型 的临床和影像学表现。确诊通常需结合酶学检测(β-半乳糖苷酶活性测定)或基因检测结果,如仍有疑问,可进一步复查酶活性和基因分析以明确。
治疗方案与康复计划
1. 治疗策略:
- 对症与支撑干预:目前主要以对症治疗为主,包括物理治疗、药物镇痛、矫形支具等,减轻关节负担和延缓关节变形。
- 手术治疗:对于重度髋关节、膝关节畸形或严重的脊柱失稳,必要时考虑截骨矫形、关节置换或脊柱固定等手术,以改善畸形、稳定关节并缓解疼痛。
- 酶替代治疗(ERT)及造血干细胞移植(HSCT):虽不能根治,但在一定程度上可能改变疾病的自然进程,目前仍处于研究或部分临床使用阶段。
- 新兴疗法:如基因治疗或小分子治疗等,尚在科研或临床试验阶段,可持续关注。
2. 康复与运动处方(基于FITT-VP原则):
- 频率(Frequency):每周3-5次的适度活动。
- 强度(Intensity):以轻-中等强度为宜,尤其在髋、膝关节面临退变或畸形时,应避免高冲击动作(如跳跃或跑步)。
- 时间(Time):每次运动时间可从15-20分钟开始,逐渐延长至30-40分钟。
- 类型(Type):以水疗(游泳或水中运动)或坐姿下的上肢抗阻练习、体操训练等为主,降低对髋膝关节的负荷。
- 进度(Progression):根据患者疼痛、关节活动度及肌力变化循序渐进。若近期有关节手术或急性期疼痛,应适当减少训练或调整动作。
- 注意事项:
1) 防止关节过度负重,选择合适的护具或支具以保护膝和髋关节。
2) 监测心肺功能和肌肉疲劳程度,避免因过度训练导致关节磨损或心肺负担过大。
3) 若出现明显疼痛或畸形加重,应及时就医或与康复科医师沟通调整运动处方。
免责声明
本报告仅为基于现有影像及临床信息的参考性分析,不能替代线下面诊或专业医生的意见。如有任何疑问或病情变化,请及时前往正规医疗机构就诊。
人类医生最终诊断
黏多糖贮积症IVB型(莫尔基奥综合征B型)