Spinal tuberculosis leading to osteomyelitis and multiple abscesses



Clinical History
30-year-old male who recently immigrated from Africa presents with progressively worsening upper back pain for the past 2 years that now radiates to his right flank. He also has been experiencing night sweats, anorexia, and weight loss recently. He denies cough or shortness of breath.
Imaging Findings
CT abdomen and pelvis with contrast revealed an enhancing fluid collection in the right psoas muscle (Figure 1) and right gluteal musculature (Figure 2). It also showed a large pre-sacral fluid collection (Figure 3). Additional findings include well-corticated osteolytic lesions of the thoracolumbar spine (Figure 4).
CT chest with contrast showed kyphosis with a T8 epicentre secondary to anterior wedging of thoracic vertebrae (Figure 5).
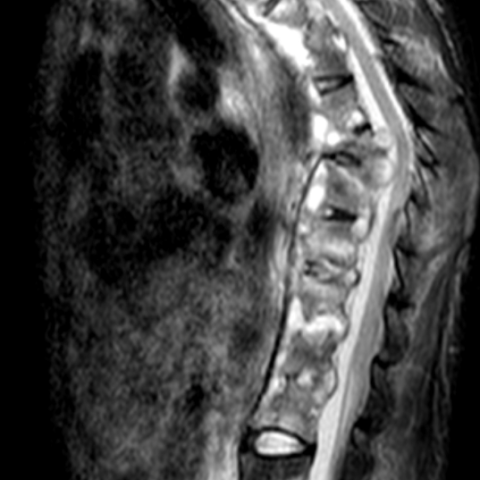
MRI lumbar and thoracic spine demonstrated extensive multisegment inflammatory process involving essentially the entire thoracolumbar spine with extensive multisegment prevertebral and paraspinal fluid collection on STIR sequence (Figure 6). It also showed a prevertebral fluid collection largest in the sacral region on STIR sequence (Figure 7).
Discussion
According to the World Health Organization, an estimated 10.6 million people became ill with tuberculosis (TB) globally in 2021, equivalent to 134 cases per 100,000 people [1]. 1.6 million died from the disease, making it the second most common infectious cause of death behind Covid-19 [1]. An estimated 3% of TB cases are extrapulmonary, with around 5% of those cases being spinal TB, also known as Pott disease [2]. This means there are likely around 16,000 cases of spinal TB every year.
Spinal TB is usually the result of haematogenous seeding to the paravertebral vessels from a primary site, such as the lungs [3]. It can present in a variety of ways depending on disease severity, with symptoms such as fever, fatigue, back pain, vertebral deformities such as kyphosis, and neurologic deficits [3]. For diagnosis, evidence of TB through various methods such as skin-testing or biopsy coupled with imaging findings is the gold standard [4].
Plain films have a low sensitivity in early stages but can show vertebral body destruction and spinal deformity in later stages. Chest x-ray is also important to look for the presence of pulmonary disease [3]. CT can show vertebral body destruction and osteolytic lesions at earlier stages than plain films [5]. MRI is the most sensitive form of imaging as it can easily detect structural abnormalities as well suspicious soft tissue findings such as oedema and spinal abscess [6].
There are 4 common MRI patterns of spinal TB: paradiscal, anterior, central, and posterior [7]. Paradiscal, which is the most common, demonstrates disc space narrowing with low signal on T1 and high on T2 with possible epidural or paraspinal abscesses [7]. Anterior shows subligamentous abscesses, preservation of the discs, and abnormal signals involving multiple vertebral segments [7]. Central includes abnormal signalling of the vertebral body with preserved disc, indistinguishable from metastasis or lymphoma [7]. Posterior is rare and includes vertebral bone erosion and associated abscess [7].
Management of spinal TB is dependent on neurologic deficits. In the absence of, systemic medical management with RIPE therapy is often adequate [4]. When deficits are present, systemic treatment along with surgical intervention such as debridement, abscess drainage – such as in this case –, and even fusion or laminectomy may be necessary [4]. With early detection and treatment, the prognosis of spinal TB is favourable [8]. This emphasises how crucial it is to detect the disease as early as possible.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Spinal tuberculosis (with osteomyelitis and abscesses)
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures






Imaging Findings
Based on the provided thoracolumbar CT and MRI images, the following features can be observed:
- Some thoracic vertebral bodies (in the mid to upper thoracic spine) show abnormal density or signal, manifesting as partial destruction of the vertebral body and blurred trabecular structures.
- The anterior margin of the vertebral body and the paravertebral region could exhibit soft tissue thickening or possible abscess formation (lower-density areas on CT and high signal on MRI T2 images), suggesting a paravertebral and possibly epidural or perispinal abscess.
- In MRI sequences, the abnormal vertebral region shows reduced T1 signal and relatively increased T2 signal, indicating active inflammation or liquefaction around the lesion.
- Some slices show mild destruction of the intervertebral disc or irregular adjacent vertebral endplates, but the exact extent of destruction requires assessment of additional imaging slices.
- No obvious extensive bony fragments or large-scale vertebral collapse are noted, but there may be a mild wedge deformity in adjacent vertebrae.
Potential Diagnoses
Considering the patient’s clinical presentation (progressive back pain, night sweats, weight loss, etc.) and the above imaging findings, the following possibilities should be taken into account:
- Tuberculous Spondylitis (Pott’s Disease): Most commonly seen in developing countries or in patients with relevant epidemiological backgrounds. Characteristic imaging includes vertebral body destruction and paravertebral or epidural abscess. It is often accompanied by systemic tubercular symptoms such as night sweats, weight loss, and fatigue.
- Bacterial (Pyogenic) Spondylitis: Primarily caused by Staphylococcus or other bacteria. It can present with vertebral destruction and soft tissue abscess, though clinically there is often a more acute onset with fever and elevated white blood cell counts.
- Fungal Spondylitis: Less common, but can cause vertebral destruction. It is typically seen in immunocompromised patients and often has a relatively slower progression.
- Vertebral Metastases or Lymphoma: Tumors may lead to vertebral destruction and local soft tissue masses. Systemic symptoms can vary depending on the primary site, and imaging findings may include multiple lesions or atypical patterns of bone destruction.
Final Diagnosis
Taking into account the patient’s age (30 years), origin from a high-prevalence region (Africa), clinical symptoms (chronic back pain, night sweats, weight loss), imaging findings (vertebral destruction with paravertebral abscess), and epidemiological background, the most likely diagnosis is tuberculous spondylitis (Pott’s disease).
If further tests related to Mycobacterium tuberculosis (e.g., tuberculin skin test, interferon-gamma release assay, ESR and CRP, pathological biopsy, etc.) confirm tuberculosis infection, the diagnosis can be established definitively.
Treatment Plan and Rehabilitation
Treatment Strategy
- Pharmacotherapy: Standard anti-tuberculosis therapy (RIPE regimen: Rifampin, Isoniazid, Pyrazinamide, and Ethambutol) usually lasts at least 6 months. In some cases, it may extend to 9 months or longer, depending on the extent of disease and treatment response.
- Surgical Intervention: In cases of spinal cord or nerve compression, significant vertebral destruction leading to spinal instability, or large abscesses, surgery may be considered. Procedures can include abscess drainage, debridement, and spinal fixation or fusion.
- Nutritional Support and Systemic Management: Individuals with tuberculosis often experience malnutrition. Ensuring sufficient protein and calorie intake is important, along with maintaining general physical recovery.
Rehabilitation and Exercise Prescription
During and after the course of treatment, rehabilitation strategies should be tailored to the level of spinal stability achieved. The following example plan should be adjusted according to individual circumstances:
-
Early Phase (Acute and Infection Control):
- Focus on rest, immobilization, and gentle exercises to avoid increased stress on the spine.
- Basic breathing exercises in bed or a seated position to improve lung function and circulation.
- Light isometric exercises for core muscles (e.g., supine abdominal draw-in, posterior pelvic tilt), if permitted.
-
Mid Phase (After Stabilization and Inflammation Control):
- Increase low-intensity strength exercises based on spinal stability. Consider small-range trunk stabilization exercises, such as bridging or partial-range back extensions.
- Protect the spine while performing light resistance training for upper or lower limbs in a seated position.
- Engaging in up to 30 minutes of low-intensity walking, swimming, or water-based exercises can help improve cardiovascular function and overall muscle strength.
-
Late Phase (Functional Reconstruction and Strengthening):
- Gradually increase exercise frequency (3-5 times per week), with each session lasting about 30-45 minutes of moderate-intensity aerobic exercise (e.g., jogging, stationary cycling).
- Incorporate resistance training for core and back muscles to maintain spinal stability and prevent reinjury.
- Adjust exercise intensity according to bone healing and overall physical recovery, closely monitoring pain and fatigue levels.
Summary of FITT-VP Principle:
- Frequency: 3-5 times per week, gradually increasing to 5-7 times per week for low-intensity activities.
- Intensity: Start with low intensity in early stages and increase to moderate intensity as recovery progresses.
- Time: Extend each exercise session from 15-20 minutes to about 30-45 minutes.
- Type: Choose forms of exercise with minimal spinal impact and full-body involvement, such as walking, swimming, or exercises using fixed equipment.
- Progression: Progress to higher intensity and more complex movements based on symptom relief, inflammation control, and bone stability.
Disclaimer
This report is a reference-based analysis solely on the provided imaging and medical history. It does not replace in-person evaluation or professional medical advice. Specific treatment decisions should be made at a qualified medical institution by an experienced physician, integrating clinical examinations and other auxiliary tests.
Human Doctor Final Diagnosis
Spinal tuberculosis (with osteomyelitis and abscesses)