Evaluation of persistent ankle pain


Clinical History
A 43-year-old white female patient was examined in the orthopaedic department because of persistent ankle pain and numbness, while standing or walking. The physical examination showed restricted movement and moderate tenderness of the medial ankle. There was neither swelling nor erythema. There was no history of previous trauma.
Imaging Findings
X-rays of the left ankle were performed, followed by MR imaging with 1.5 Tesla scanner using standard sequences.
The AP and oblique radiographs of the ankle showed no abnormalities (not shown).
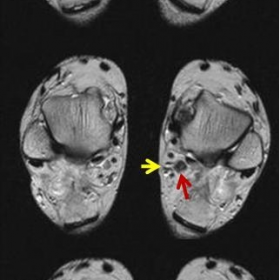
The axial T2-w TSE MR images (Fig. 1) show the flexor digitorum accessorius longus (FDAL) muscle coursing posteromedial to the flexor hallucis longus and abutting the neurovascular bundle. The accessory muscle originates from the flexor hallucis longus muscle. The coronal T1-w MR image (Fig. 2) shows the flexor digitorum accessorius longus muscle medial to the calcaneal bone.
Discussion
A. The FDAL muscle is seen in about 7% of the general population, more often in men and in about 12% of patients with a clinical diagnosis of tarsal tunnel syndrome [1, 2]. Its origin varies and includes the tibia, fibula or any structure in the posterior compartment [3]. The FDAL tendon has a course within the tarsal tunnel in close proximity to the posterior tibial artery and tibial nerve [1]. Distally, the tendon inserts either onto the quadratus plantae muscle or the flexor digitorum longus tendon [1, 2]. The close relationship of the FDAL with the posterior tibial nerve may explain its association with the clinically diagnosed tarsal tunnel syndrome [4].
B. The usual clinical presentation is ankle pain or/and numbness. Mass effect could be the pathophysiologic mechanism. Radiologists have to include in the list of differential diagnosis those entities that cause symptoms compatible with tarsal tunnel syndrome. In this respect, a careful clinical examination and access to the history of the patient are important before performing imaging.
C. The FDAL is depicted on axial MR images, located in the tarsal tunnel deep to the neurovascular bundle [3]. Its signal intensity follows that of the surrounding muscles in all pulse sequences. Coronal images (Fig. 2), are important in assessing the lack of calcaneal insertion which is seen in other accessory muscles within the tarsal tunnel, such as peroneocalcaneus internus and tibiocalcaneus internus [3].
D. MRI is the imaging method of choice in the differential diagnosis of the entities that cause tarsal tunnel syndrome, and is able to suggest the presence of an FDAL. Therefore, MRI contributes to early diagnosis and accurate treatment planning of this rare entity.
E. An accessory muscle may be the cause of tarsal tunnel syndrome. The delayed onset of symptoms of a congenital lesion may be related to modified activities, i.e. sports or profession-related. MRI is the gold standard for diagnosis and treatment planning.
Differential Diagnosis List
Final Diagnosis
Flexor digitorum accessorius longus muscle
Liscense
Figures
Axial T2-w TSE MR images

Coronal T1-w MR image

Imaging Findings
In the provided ankle MRI images, an additional tendon/muscle belly structure can be observed near the medial malleolus (suspected to be an accessory muscle of the flexor hallucis or flexor digitorum longus, commonly referred to as “Flexor Digitorum Accessorius Longus, FDAL”). This structure is in close proximity to the posterior neurovascular bundle, located on the posteromedial side of the talus. Its signal intensity is similar to that of the surrounding muscle tissue, with no obvious swelling or significant effusion. There is no apparent bony damage or fracture in the tibia, talus, and other key bones. The overall soft tissue shows no significant edema, and surrounding ligaments appear relatively intact.
Potential Diagnoses
- Tarsal Tunnel Syndrome: Due to the accessory muscle (FDAL) occupying space in the tarsal tunnel, it may compress the tibial nerve or its branches, causing medial ankle pain, numbness, and related clinical symptoms.
- Other Causes of Tarsal Tunnel Narrowing: For example, ganglion cysts, hemangiomas, schwannomas, or variant tendons may also lead to local nerve compression.
Final Diagnosis
Considering the patient’s chronic ankle pain and numbness, along with the clear imaging findings showing an accessory muscle (FDAL) adjacent to the posterior neurovascular bundle, the most likely diagnosis is “Tarsal Tunnel Syndrome caused by the accessory muscle.”
Treatment Plan and Rehabilitation
Treatment Strategy:
1. Conservative Management:
- Ensure adequate rest and reduce prolonged standing or walking. Consider using ankle supports or arch supports to alleviate pressure.
- Under the guidance of a specialist, use nonsteroidal anti-inflammatory drugs (NSAIDs) or other analgesics to relieve pain and inflammation.
- Physical therapy such as ultrasound, heat therapy, and manual release techniques can help relieve pressure in the tarsal tunnel.
- If conservative treatment proves ineffective or symptoms persist or worsen, surgical decompression and, if necessary, removal or adjustment of the accessory muscle (FDAL) may be considered.
Rehabilitation Exercises and Exercise Prescription (FITT-VP Principle):
-
Initial Phase:
- Frequency: 3 times per week.
- Intensity: Low intensity, recommended lower-limb weight-bearing exercises (e.g., short-distance walking with assistance) without inducing significant pain.
- Time: Approximately 10–15 minutes per session.
- Type: Ankle range-of-motion exercises (dorsiflexion/plantarflexion, circular movements) and simple foot muscle strengthening exercises (e.g., towel-grab exercises).
- Progression: Gradually increase each session to around 20 minutes as pain and numbness improve.
-
Intermediate Phase:
- Include standing balance training and mild resistance exercises (e.g., resistance band eversion and inversion), focusing on ankle sensitivity and nerve mobilization.
- Depending on progress, consider adding one more session per week or extending each session by about 5 minutes.
-
Late Phase:
- Strengthen the ankle and foot muscles, gradually add low-impact aerobic activities (e.g., brisk walking, elliptical training) to improve overall lower-limb function.
- Regularly re-evaluate and seek medical advice if significant pain or numbness worsens.
- Monitor changes in ankle pain and numbness closely. If symptoms worsen, reduce or discontinue exercises and seek medical assessment promptly.
- For patients with osteoporosis or compromised lower-limb circulation, an individualized plan under professional supervision is recommended with careful monitoring.
Disclaimer
This report provides a reference analysis based on existing imaging and clinical information and cannot replace in-person consultation or the diagnosis and treatment recommendations of professional medical institutions. Patients should follow the guidance of professional physicians to further refine their diagnosis and treatment plan.
Human Doctor Final Diagnosis
Flexor digitorum accessorius longus muscle