A pseudotumour due to moderate metal-on-metal disease in a patient with a metal-on-metal total hip replacement



Clinical History
64-year-old woman, former professional ballet dancer, presented for routine check-up after bilateral total hip replacements. The right hip was operated on 4 years ago and the left hip was operated on one year ago. Physical examination showed a healthy woman with a good range of motion of both hips.
Imaging Findings
Radiograph of the pelvis shows a metal-on-metal total hip replacement on the right side and an uncemented total hip replacement on the left side. Ultrasound of the right hip region shows a large collection in the soft tissues around the right hip with a fluid-debris level. No internal vascularization visible on colour Doppler. MRI shows a periprosthetic fluid-filled cavity with a diameter of more than 5 cm maximum diameter, a ‘fluid-fluid level’, and no oedema in the surrounding tissues.
Discussion
Background:
In the 1990s second generation metal-on-metal hip replacements were introduced [1]. Metal-on-metal hip replacements were marketed as the solution for young and active patients because the expected long life expectancy of the metal-on-metal hip replacements due to minimal wear should result in a reduction of the expected number of revisions needed over a life time [2, 3].
Clinical perspective:
However, national joint registries in the UK and in Australia showed an unacceptable high revision rate [4]. Furthermore, exceptionally high levels of cobalt ions were measured in the blood of some patients with metal-on-metal hip replacements [5, 6]. The problem with metal-on-metal hip replacements is likely caused by metal debris which could result in high concentrations of metal ions in the blood and in locally adverse soft tissue reactions [1] also called pseudotumour, ALTS (Adverse Local Tissue Reaction), and ARMD (Adverse Reaction to Metal Debris). Histopathology shows an aseptic lymphocyte-dominated vasculitis-associated lesion (ALVAL) [3].
Imaging perspective:
In 2011 Anderson et al published a grading system for the severity of soft tissue changes associated with metal-on-metal hip replacement on MR [2]. Grade A: normal post-operative appearances including seromas and small haematomas. Grade B: fluid-filled cavity with high signal T2 wall; inflammatory changes in the soft tissues. Grade C1 (mild Metal-on-Metal Disease): periprosthetic soft tissue mass with no hyperintense T2-weighted fluid signal or fluid-filled peri-prosthetic cavity; either less than 5 cm in maximum diameter. Grade C2 (moderate Metal-on-Metal Disease): periprosthetic soft tissue mass/fluid-filled cavity greater than 5 cm diameter or C1 lesion with either of the following (1) muscle atrophy or oedema in any muscle other than short external rotators or (2) bone marrow oedema (hyperintense on STIR). Grade 3 (severe Metal-on-Metal Disease): any of the following (1) fluid-filled cavity extending through deep fasci, (2) a tendon avulsion, (3) intermediate T1-weighted soft tissue cortical or marrow signal, (4) fracture.
Teaching points:
The prevalence of pseudotumour formation in patients with a metal-on-metal hip replacement, i.e. total hip arthroplasty or hip resurfacing arthroplasty, has been reported in up to 71% of patients [1, 7]. However, the presence of symptoms does not seem to correlate with the presence or the size of a pseudotumour [1].
Differential Diagnosis List
Final Diagnosis
Pseudotumour due to moderate metal-on-metal disease.
Liscense
Figures
Radiograph of the pelvis

Ultrasound of the right hip

MRI of the right hip
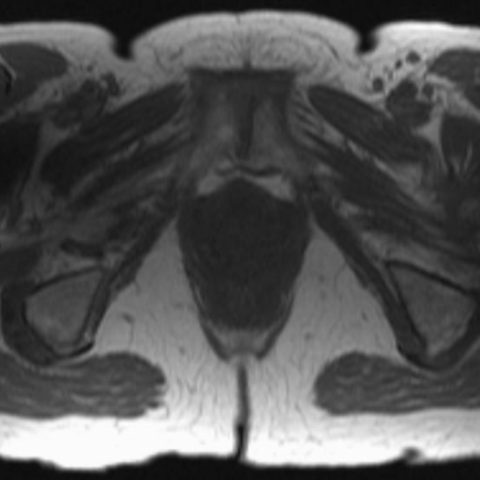
MRI of the right hip

MRI of the right hip

MRI of the right hip

1. Radiological Findings
Based on the provided bilateral hip joint X-ray, ultrasound, and MRI images, the following observations are made:
- Bilateral hip joint replacements are in place, with overall stable prosthetic positioning. No obvious loosening or severe osteolysis.
- No significant large-scale bone resorption or fracture lines noted.
- On the left hip, ultrasound and MRI reveal certain soft tissue changes around the joint, indicating a possible small fluid or mixed density/signal shadow. The lesion appears relatively regular with a clear boundary, which may correlate with post-operative changes or mild bursitis/serous cavity. However, vigilance regarding a metal-on-metal prosthesis-related pseudotumor is advised.
- No apparent extensive muscle edema or severe tendon detachment is observed.
2. Potential Diagnoses
Based on the patient’s history of metal-on-metal hip replacement and current imaging findings, consider the following differential diagnoses:
- Metal-on-metal prosthesis-related pseudotumor (Pseudotumor, ALVAL)
Due to metal debris or ions generated by metal wear, local soft tissue may form pseudotumors or aseptic inflammation (ALVAL). Radiologically, pseudotumors typically appear as fluid-filled or cystic soft tissue lesions around the joint, with high or mixed signal intensity on T2 MRI. - Postoperative routine fluid accumulation or bursae thickening
Some postoperative patients may exhibit small effusions or thickened bursae, which are not necessarily pathological, especially if they are minor, localized, or asymptomatic. Clinical follow-up is recommended. - Asymptomatic, stable postoperative changes
Scar tissue, fibrosis, or minimal effusions may occur postoperatively. If the patient has no significant symptoms and maintains good hip joint mobility, these could represent normal postoperative findings.
3. Final Diagnosis
Taking into account the patient’s age, history of bilateral metal-on-metal hip replacement, and current imaging features, the most likely diagnosis is:
“Suspected metal-on-metal hip prosthesis-related pseudotumor”
Given that the patient currently exhibits mild symptoms, good range of motion, and no significant muscle destruction or large-scale bone changes, it is recommended to regularly follow up the serum metal ion levels (e.g., cobalt, chromium) along with imaging to monitor the lesion’s progression. If the pseudotumor expands or symptoms worsen, more aggressive intervention or revision surgery may be warranted.
4. Treatment Plan & Rehabilitation
- Treatment Strategy
- Conservative treatment and close observation: For patients with minimal pain and acceptable function, conservative management is preferred. This includes regular follow-up (blood metal ions, imaging tests) and symptomatic relief measures.
- Medication: In cases of local inflammatory reactions or mild pain, non-steroidal anti-inflammatory drugs (NSAIDs) can be used under medical guidance for symptom control.
- Criteria for surgical intervention: If significant pain, rapid tumor growth, impaired joint function, or marked elevations in metal ion levels are observed, further surgical management should be considered. Procedures may include debridement and removal of the lesion or revision arthroplasty.
- Rehabilitation & Exercise Prescription
Since the patient has a background in dance and a high baseline of physical activity, it remains crucial to tailor a gradual, individualized exercise program considering the bilateral hip prostheses:
- Initial Phase (FITT-VP principle)
- Type: Focus on joint flexibility training, core muscle stabilization exercises, and light resistance workouts. Aquatic aerobic exercises may be added to reduce hip joint stress.
- Frequency: 2–3 times per week, depending on tolerance.
- Intensity: Low to moderate intensity, avoiding prolonged or extreme squatting and twisting maneuvers.
- Time: Approximately 30 minutes per session, possibly in segments. Take breaks or reduce duration if fatigue or hip discomfort occurs.
- Progression & Volume: Gradually increase range of motion and resistance based on joint stability and a pain-free range. Adjust slightly every 2–4 weeks as tolerated.
- Intermediate Phase
- If no complications arise and pain is controllable, slowly increase walking or stationary cycling duration to 40–50 minutes per session.
- In collaboration with a physical therapist or rehabilitation specialist, incorporate core strengthening and lower extremity stabilization exercises, such as light squats or lunges, while closely monitoring hip reactions.
- Advanced Phase
- If hip mobility remains unrestricted and imaging follow-up shows no significant deterioration, low-impact dance movements or balance training on mats may be gradually introduced to preserve flexibility and professional skills.
- Consistently monitor for hip pain or post-exercise discomfort. If an acute exacerbation occurs, promptly evaluate and reduce activity intensity.
- Special Considerations
- Regularly assess bone density and muscle strength to minimize fall risk.
- Thoroughly warm up the hips and lower limbs before each session and perform adequate stretching afterwards.
- Engage the medical team (orthopedic surgeon, rehabilitation specialists) to continuously monitor hip alignment and prosthesis stability.
- Initial Phase (FITT-VP principle)
In summary, based on the current imaging findings and the patient’s good clinical status, we recommend regular follow-up and moderate functional exercises. If any significant symptoms develop or the lesion appears to progress, a second imaging evaluation and further intervention should be promptly considered.
Disclaimer: This report is a reference analysis based on the available clinical and imaging data. It does not replace in-person consultation or professional medical advice. If you have any concerns or if your condition changes, please seek medical attention promptly.
Human Doctor Final Diagnosis
Pseudotumour due to moderate metal-on-metal disease.