Synovial sarcoma: The diagnostic challenge of a sarcoma mimicking a benign tumour



Clinical History
A 24-year-old male patient with no prior medical history consulted because of lower back pain. Clinical evaluation revealed left sacral swelling that was painful on palpation.
Imaging Findings
An ultrasound of the left para-spinal region was performed showing a hypoechogenic lesion with subtle peripheral calcifications visible as a hyperechoic linear structure of the superficial component of the lesion (Figure 1). There was no hyperemia at Doppler.
A CT examination was performed and confirmed the presence of peripheral calcifications. (Figure 2).
MRI showed a well-delineated, lobulated lesion with a hyperintense T1 and T2 signal and homogenous enhancement (Figure 3, 4, 5). Peripheral calcifications confirmed by the CT were hypointense on T2 (Figure 3). The lesion measured 2.5 x 1 x 4 cm and was situated within the para-spinal muscles with a subcutaneous extension at the level of S3, in a dumbbell form (Figure 3).
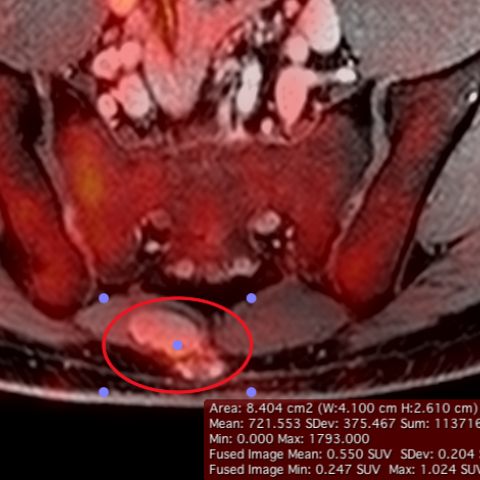
There was no significant hyper-metabolism of the lesion with a SUV-max 0f 1.0 on the PET-MRI (Figure 6).
Surgical removal of the lesion revealed a malignant tumour with the translocation t(X-18) of the SYT and SSX2 genes.
Discussion
Synovial sarcoma is a malignant tumour that represents 8-10% of all sarcomas affecting adults aged from 15-50 [1, 2]. The majority of lesions occurs in the extremities and is most commonly situated in the lower extremities especially in the popliteal fossa [1, 2]. Histologically, synovial sarcoma does not originate from synovial cells despite its name and is usually not located within a joint. Synovial sarcoma poses a diagnostic challenge due to its indolent course and seemingly benign imaging characteristics with slow growth and small size (<5cm on initial presentation) leading to an average time to diagnosis of 2-4 years [2]. Patients usually present with a palpable soft-tissue mass that is slow growing. Pain and tenderness are frequent [2].
Radiography is often the initial examination but is normal in 50% of cases [1]. Imaging may show a lobulated soft-tissue mass with calcifications in 30% of cases, often eccentric or peripheral [1, 2]. Periosteal reaction is observed in 20% of patients. Aggressive bone invasion and destruction are uncommon [2].
CT is useful to depict calcifications and to determine bone invasion or periosteal reaction. Findings are non-specific and show a well-defined soft-tissue mass usually found near a joint.
MRI is the modality of choice because of excellent tissue contrast enabling to depict the extent of the lesion. 91% of patients present with a well-defined lesion with rounded or lobulated margins [1]. The tumour displays a heterogeneous intermediate signal on T1-weighted images and high signal on T2-weighted images. Lesions may bleed and lead to high T1-signal due to methaemoglobin. Cystic components are seen in 77% of patients [1]. Approximately one third of lesions demonstrate the “triple signal pattern” which translates different signal intensities due to cystic, fibrous and tissue components [1]. Lesions show enhancement that is more commonly heterogeneous but may be homogeneous in up to 17% of cases [2].
Nuclear imaging does not play a significant role in the workup of synovial sarcoma but may be used in the evaluation of metastases or recurrent disease and in targeting biopsies. PET imaging demonstrates increased tracer accumulation with high standard uptake values being predictive for overall survival in various studies [2, 3].
Treatment of the lesion is achieved with surgery. Chemotherapy may be used in cases of metastatic, most commonly to the lung, or residual disease. Radiation therapy plays a role in the treatment of marginally resected tumours [2]. 5-year survival rates range from 36%-76% [2]. A favourable prognosis is expected in patients with a tumour size <5cm [4].
Differential Diagnosis List
Final Diagnosis
Synovial sarcoma
Liscense
Figures
CT examination

MRI

PET-MRI
MRI

Ultrasound

MRI

Imaging Findings
Based on the imaging studies provided by the patient (CT, MRI, and ultrasound), the following key features are observed:
- The lesion is located on the left side of the sacrum, appearing as a soft tissue mass with relatively clear margins. Some areas present lobulated or round-like contours.
- On CT, a soft tissue density mass is seen. In some regions, small spotty or eccentrically distributed calcifications are visible. There is minimal bone reaction but no significant bone destruction.
- MRI shows an iso- to slightly hypointense signal on T1-weighted images and a hyperintense signal on T2-weighted images. Local cystic or hemorrhagic components may be observed, along with a possible “triple signal” appearance.
- The mass has relatively clear demarcation from surrounding tissues and exerts local pressure or displacement on adjacent soft tissues. No evident invasion into the joint cavity is noted.
- Ultrasound images indicate both solid and cystic components within the mass, with moderate to high blood flow signals.
- PET-CT assessment shows regions of moderate to high metabolic activity within the mass.
Potential Diagnoses
Considering the patient’s age (24 years), lower back pain, a palpable mass, and the imaging characteristics, the following diagnoses should be taken into account:
- Synovial Sarcoma
- Commonly seen in young to middle-aged adults (15–50 years old) and classified as a soft tissue sarcoma.
- The tumor typically grows slowly, with mild or nonspecific early symptoms, often mistaken for benign lesions.
- Imaging may reveal a lobulated soft tissue mass, sometimes with calcifications. MRI often shows heterogeneous signals and a “triple signal” pattern.
- Neurilemmoma (Schwannoma) or Other Soft Tissue Tumors
- Schwannomas can also appear as soft tissue masses with mixed MRI signals.
- They are often closely associated with nerve pathways and may present with neurological symptoms.
- Other Soft Tissue Sarcomas or Cystic-Like Lesions
- Examples include liposarcoma, leiomyosarcoma, or cystic teratoma. However, these typically occur in specific locations or exhibit other characteristic imaging findings.
These are the main differential diagnoses and should be confirmed by histopathological evaluation (biopsy).
Final Diagnosis
Taking into account the patient’s age, symptoms, imaging findings (local calcifications, small cystic components, “triple signal” on MRI), as well as the slow-growing clinical nature, the most likely diagnosis is Synovial Sarcoma.
Definitive diagnosis depends on pathological evaluation (core needle biopsy or intraoperative frozen section). Wherever feasible, specific gene markers (e.g., t(X;18) translocation) can also be used to confirm the diagnosis.
Treatment and Rehabilitation Plan
1. Treatment Strategy:
- Surgical Treatment: Most synovial sarcomas require surgical resection to achieve complete removal of the tumor with adequate margins.
- Chemotherapy and Radiotherapy:
- When there is a risk of residual disease postoperatively or when there is a risk of distant metastasis, adjuvant radiotherapy or chemotherapy may be considered.
- Radiotherapy can be beneficial, particularly in cases of marginal resection or a high risk of local recurrence.
- Follow-up and Monitoring: After surgery, regular imaging follow-ups (MRI or CT) are essential to monitor for recurrence or metastasis, especially pulmonary metastases.
2. Rehabilitation and Exercise Prescription Suggestions:
- Preoperative Rehabilitation: If preoperative treatment or a waiting period is required, low-intensity exercises for core and lower limb muscles can help maintain overall strength. High-impact or intense activities should be avoided to reduce local pain and irritation to the tumor.
- Early Postoperative Rehabilitation:
- During the first 1–2 weeks after surgery, the primary goals are pain relief and wound healing. Light bed-based or seated activities, such as ankle pumps and deep breathing exercises, are recommended.
- If the wound condition allows and there are no significant complications, gradual progression to gentle active lower limb movements can be initiated under professional guidance. Excessive stretching should be avoided to protect the surgical site.
- Mid-to-Late Rehabilitation (3–6 weeks post-surgery):
- Frequency (F): 3–4 times per week.
- Intensity (I): Begin with low intensity (e.g., 30–40% of maximum muscle strength) and increase gradually as pain and function improve.
- Time (T): 20–30 minutes per session, divided if needed, depending on tolerance.
- Type (T): Exercises may include core training in seated or supine positions, light resistance exercises, and stability drills such as wall-sits. If tolerated, transition to low- to moderate-impact aerobic activities (e.g., elliptical machine, stationary bike).
- Volume and Progression (–VP): Adjust volume incrementally based on patient tolerance, prioritizing proper form and safety. Discontinue or modify if significant pain or swelling occurs, and consult a specialist promptly.
- Special Considerations: In cases of bone involvement or other functional limitations, protect the affected area during rehabilitation to avoid excessive load leading to new injuries or stress fractures.
Disclaimer:
This report is based on the current imaging and clinical information for reference only. It cannot replace in-person consultation or individualized medical advice from a professional physician. If you have any questions or if symptoms worsen, please seek medical attention promptly for an accurate diagnosis and treatment recommendations.
Human Doctor Final Diagnosis
Synovial sarcoma