Paget disease of the patella



Clinical History
A 59-year-old woman presented to the orthopaedics outpatient clinic of our hospital due to complaints of swelling and pain anteriorly of the left knee since three years. Movement of the knee was not impaired. The patient’s mother had morbus Paget, the family history was otherwise unremarkable.
Imaging Findings
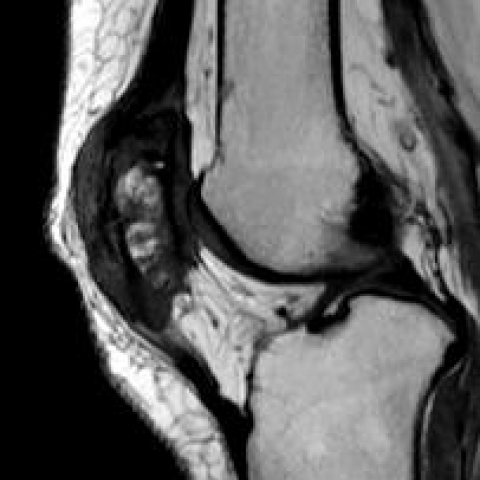
A CT and gadolinium enhanced MRI were performed. CT showed a diffusely enlarged patella, with coarse bone trabeculae and cortical thickening. Centrally in the patella there were several small sclerotic and lytic focal areas. (Figures 1 and 2). On MR images the thickened cortex was iso-intense on T1, had a high signal intensity on T2-weighted images, and enhanced strongly after gadolinium. Centrally, the lesion had mixed signal intensities on MRI. The patellar lesion did not extend into the surrounding soft tissue. Retropatellar chondropathy was present. (Figures 3-6)
Discussion
BACKGROUND
Paget disease (PD) is a bone metabolic disorder with a disturbed osteoblast and osteoclast equilibrium that changes bone architecture.[1] The disease was first described in 1877 by Sir James Paget, and it was called “osteitis deformans” at the time. The epidemiology of PD appears to be changing rapidly: several groups in different parts of the world reported a marked reduction in the prevalence and incidence of PD, as well as in the severity of disease seen by clinicians. These findings seem most likely to be caused by changes in exposure to (partly still unknown) environmental factors that have a role in the development of PD.[1] However, paramyxovirus has been put forward as a possible infectious cause.[2] Genetic factors are also important: mutations in SQSTM1 occur in 25-50% of familial PD.[1] The disease incidence increases with age, and the male to female ratio is 2:1. Three phases are described in PD: the first being an osteolytic phase (“hot” phase), the second a mixed lytic and blastic phase, and the third a sclerotic phase. Typically, bone expansion, cortical thickening and trabecular bone thickening are present in the second phase. In 1% of patients, a malignant transformation to osteosarcoma or giant cell tumour can take place. Treatment with biphosphonates can be applied to decrease the osteoclast activity and bone resorption.
[2]
The most affected bones in PD are the skull, spine, pelvis and femur. Usually the disease is polyostotic. When only one bone is affected, this type is called monostotic PD. PD of the patella is very rare. It has been previously described in a review by Ploumis et al. [3] To our knowledge, there have been 4 case-reports previously published on the topic.[4-7]
OUTCOME
After the MRI and CT had been done, a CT-guided biopsy was performed to confirm the radiological suspicion of PD (Figure 7). Pathology showed coarsening of the bone trabeculae, an increased number of osteocytes and focally increased osteoblastic activity. The diagnosis of a “Paget-like reaction” with a differential diagnosis including PD, posttraumatic changes or changes due to an inflammatory reaction was made. The patient had experienced a trauma several years ago. To clarify the diagnosis, a total body bone scintigraphy was performed which showed intense increased uptake of the radiopharmacon (99 Technetium) by the left patella without other suspect lesions, (Figure 8) consistent with PD.
Differential Diagnosis List
Final Diagnosis
Morbus Paget of the patella
Liscense
Figures
Sagittal CT image of the left knee.

Axial CT image of the left knee.

Sagittal T1 Gadolinium enhanced MR image.

Axial T1 Gadolinium enhanced MR image.

Axial T2 SPAIR image.

CT guided biopsy image (axial).

Bone scintigraphy AP (left) and PA (right) image.

Sagittal T1 MR image of the left knee.
I. Imaging Findings
Based on the provided CT and MRI images, the patient’s left patella demonstrates a mixed pattern of osseous changes, showing both radiolucent (osteolytic) and sclerotic areas, along with focal cortical thickening. On MRI, the lesion exhibits abnormal signal intensity with uneven signal on both T1 and T2 sequences, suggesting disordered and thickened trabecular architecture. No obvious soft tissue mass or significant synovial thickening within the joint cavity is noted. The adjacent femoral distal end and tibial proximal articular surfaces appear uninvolved. Bone scintigraphy shows markedly increased radiotracer uptake in the left patella, with no similar findings in other regions.
II. Potential Diagnoses
- Bone Paget’s Disease (Paget’s Disease)
Reason: The patient has a family history (the mother had Paget’s disease), and imaging shows a mixture of osteolytic and sclerotic changes in the patella. Bone scan reveals high uptake, and the lesion is solitary, matching the features of monostotic Paget’s disease. - Post-Traumatic or Inflammatory Reaction
Reason: Histopathological findings indicate a “Paget-like reaction,” which may be related to past local trauma or an inflammatory reactive change. However, the single affected skeletal site with high uptake and chronic symptoms aligns more closely with Paget’s disease. - Other Rare Primary or Secondary Bone Tumors (e.g., Giant Cell Tumor)
Reason: Some bone tumors can also present with osteolysis or mixed-density lesions. However, the overall course and the pattern of adjacent structural involvement do not fully correspond to these conditions, and pathology also suggests “Paget-like” changes.
III. Final Diagnosis
Considering the patient’s age, family history, clinical symptoms, CT and MRI features, the bone scan results showing significant radiotracer uptake only in the patella, and the pathological hint of “Paget-like change,” there is a high suspicion of monostotic Paget’s disease of the patella. After ruling out other tumors or post-traumatic changes, the most likely diagnosis is monostotic Paget’s disease of the patella.
IV. Treatment Plan and Rehabilitation
Treatment Strategy:
- Medication: For patients with symptoms or significantly elevated laboratory findings (e.g., alkaline phosphatase), considering bisphosphonates (such as alendronate, risedronate) can help suppress osteoclast activity and reduce bone destruction and deformity. Anti-inflammatory and analgesic drugs may be used to relieve pain as appropriate.
- Surgical Intervention: If there is severe deformity, joint dysfunction, or suspicion of malignant transformation, surgical treatment such as curettage, internal fixation, or joint replacement may be considered. However, given that the patient’s knee joint mobility is currently unaffected, surgery is not necessary at this stage.
- Regular Follow-Up: Periodic follow-up imaging and monitoring of relevant laboratory indicators are recommended, especially alkaline phosphatase levels.
Rehabilitation and Exercise Prescription:
- Early Stage (Stable Symptoms):
• Focus on protecting joint function and alleviating discomfort. Engage in low-load range-of-motion exercises for the knee, such as mild flexion and extension in a sitting or supine position, 1–2 times a day, for 10–15 minutes each time.
• Combine with local physiotherapy, hot compresses, or small-range muscle strength exercises, avoiding excessive weight-bearing. - Middle Stage (Symptom Improvement, Good Range of Motion):
• Gradually increase the range of knee flexion and extension as long as it does not exacerbate pain. You may use resistance bands or light weights (e.g., 0.5–1 kg) for isometric quadriceps contraction and resistance training, 2–3 times a week, 15–20 minutes each session.
• Add low-impact aerobic activities such as flat-ground walking or cycling for 20–30 minutes each session, 3–5 times a week, maintaining a moderate to low intensity. - Late Stage (Functional Enhancement):
• If knee joint strength and stability are adequate, incorporate closed-chain exercises (e.g., partial squats, sit-to-stand training). Carefully monitor for pain and joint reactions.
• Maintain at least three weekly sessions of both aerobic and resistance exercises, gradually increasing intensity and duration based on individual recovery.
Throughout rehabilitation, follow a gradual, individualized approach (FITT-VP: Frequency, Intensity, Time, Type, Progression, and Personalization) and continuously monitor pain or other discomfort. If joint swelling, significant pain, or restricted motion occurs, seek medical evaluation promptly.
V. Disclaimer
This report is based on the provided information for clinical reference only. The specific diagnosis and treatment plan require comprehensive in-person evaluations and the advice of a professional physician. This report does not replace regular medical services. In case of any doubts or changes in condition, please consult a doctor promptly.
Human Doctor Final Diagnosis
Morbus Paget of the patella