


Clinical examination of a 47-year-old male with increasing pain showed right supraspinatus (SSp) and infraspinatus (ISp) moderate atrophy. No history of trauma was reported.
Magnetic resonance imaging of the right shoulder was performed in a magnet of 1.5 Tesla. Images through axial, coronal-oblique and sagittal-oblique planes were acquired with T1, T2, T2 FAT SAT, Proton Density (DP) FAT SAT and 3D DP Cube weighing.
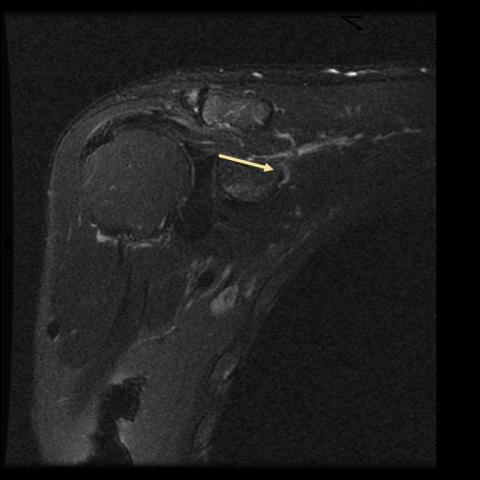
The course of the suprascapular nerve appeared enlarged, focally convoluted and slightly hyperintense at the scapular notch (Figure 1), but no signal alteration at the superior transverse scapular ligament (STLS) was reported (Figure 2). Muscular oedema (Figure 3) and grade II atrophy of the infraspinatus were observed (Figure 4). Paralabral cysts and other occupying-space lesions were excluded.
Background & Clinical Perspective
The suprascapular nerve is a mixed nerve arising from the superior trunk of the brachial plexus. It leads efferent fibres for the motor supply of supraspinatus and infraspinatus muscles and receives afferent fibres for shoulder sensitivity. Distally, the nerve traverses the suprascapular notch, a fibro-osseous tunnel bridged by the STSL [1], and it releases the supraspinatus branches. Then it directs to the root of the scapula’s spine, through the spinoglenoid notch, giving the two terminal branches for the infraspinatus. Suprascapular neuropathy at the suprascapular notch is a rare condition, often related to a paralabral cyst, it is rarely sustained by STSL thickening or ossification.
Signs and symptoms of neuropathy include aching or burning pain. The persistence of the condition may lead to paralysis. Rare painless cases have been reported when a severe clinical frame of denervation is observed [2].
Imaging Perspective
Nerve enlargement with increased T2 signal at the MRI imaging is considered an abnormal appearance [3].
The anatomic pattern of muscular oedema is significant since the involvement of both SSp and ISp (Figure 3) suggests a proximal injury [4], while isolated ISp oedema and/or atrophy typically occur with a more distal injury [5]. Adipose infiltration of supraspinatus is classified through the occupational ratio of the cross-sectional area of the SSp muscle to the SSp fossa [6], grading atrophy as mild (≥ 60%), moderate (30–59%) and severe (≤ 30%) [7].
Outcome
Isolated suprascapular neuropathy is initially treated with nonsteroidal anti-inflammatory and physiotherapy. If the compression is sustained by a cyst, ultrasound-guided nerve decompression is recommended [8]. However, surgery is warranted when there is extrinsic nerve compression or progressive symptomatology [9].
In our case, the surgeon arthroscopically practised the STS–ligament section and assessed the shape and course of the suprascapular nerve and ligament, but no macroscopical changes were observed. After six months, 75% of the shoulder’s strength was restored at the clinical follow-up.
Take Home Message / Teaching Points
In suspected suprascapular neuropathy, pathological MRI appearance such as convoluted and enlarged nerve and muscular oedema can confirm the diagnosis. The radiologist should also detect the cause of the compression when apparent and should assess the severity of the condition. Early detection can change the prognosis.
Written informed patient consent for publication has been obtained.
Suprascapular neuropathy sustained by nerve entrapment at the supra-scapular notch, non-ossified STSL
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.









Patient Information: Male, 47 years old, chief complaint of gradually worsening right shoulder pain. Clinical examination reveals moderate atrophy of the supraspinatus (SSp) and infraspinatus (ISp) muscles, with no obvious history of trauma.
Based on MRI imaging (including T2-weighted sequences):
Based on simultaneous involvement of both supraspinatus and infraspinatus muscles, along with evidence of local nerve thickening and T2 hyperintensity at the suprascapular notch, this presentation most strongly suggests suprascapular nerve entrapment leading to neuropathy.
Although the patient has atrophy in the supraspinatus and infraspinatus, there is no obvious tendon rupture or tear on imaging. If nerve pathology were ruled out, chronic tendinopathy should be considered. However, no typical large-scale tear was evident on MRI, so this possibility is relatively low.
Subacromial bursal effusion or labral cysts can compress the suprascapular nerve sheath. If a cystic lesion were visible on MRI, one would highly suspect this cause. However, the current imaging description does not indicate any obvious cystic lesion.
Considering the patient’s age, progressively worsening shoulder pain, the clinical findings of moderate supraspinatus and infraspinatus muscle atrophy, and MRI findings suggestive of signal changes in the suprascapular nerve area, the most likely diagnosis is:
“Suprascapular Neuropathy”
Further investigations may include electromyography (EMG) and nerve conduction velocity (NCV) tests to confirm the level of nerve entrapment. Arthroscopy or ultrasound evaluation may be needed to check for small cysts or ligament thickening.
Under the guidance of a professional therapist, conduct passive range-of-motion exercises for the shoulder, muscle strengthening regimens, and postural correction. Supplemental therapies such as ultrasound, heat application, or shockwave therapy can help reduce local inflammation.
Rehabilitation exercises should follow the FITT-VP principles (Frequency, Intensity, Time, Type, Progression, and Individualization):
Example exercises (for reference only):
These rehabilitation exercises should be adapted to daily feedback on pain and range of motion, avoiding excessive fatigue or pain. If discomfort or symptoms worsen, consult a physician or therapist promptly.
Disclaimer: This report is a reference-based analysis derived from current imaging and information. It is not a substitute for in-person consultations or professional medical advice. The specific diagnosis and rehabilitation plan should be formulated by a specialist according to the patient's actual condition.
Suprascapular neuropathy sustained by nerve entrapment at the supra-scapular notch, non-ossified STSL