


A 43-year-old patient, known for two surgically treated melanomas with negative follow-ups, presented with worsening chronic fatigue. His medical history included the excision of a schwannoma in the right iliac region 14 years ago. His family history was unremarkable.
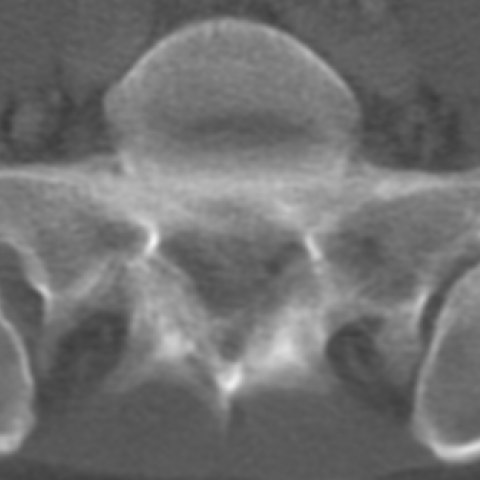
A total-body CT examination ruled out melanoma recurrence. However, it incidentally showed a hypo-dense lesion centred on the right sacro-iliac joint with adjacent bone erosion, enclosed by a sclerosis rim. Retrospectively, the lesion was found on previous CT images proving its slow evolution over a 10-year period.
A MRI confirmed the sacro-iliac joint lesion. In addition three smaller lesions were found: one in the right para-vertebral muscle at the L5 level and two adjacent to the right postero-superior iliac spine. All the lesions were iso-intense to muscle on T1 sequence and hyper-intense on STIR sequence. Hypo-intense spots on T2* sequence were present in the sacro-iliac joint lesion, theoretically suggesting calcifications or haemosiderin deposits. Gadolinium injection showed homogeneous enhancement of all the lesions.
A CT-guided biopsy of the sacro-iliac joint lesion and of the para-vertebral muscle lesion yielded the histological diagnosis of schwannoma.
Schwannomas are benign tumours arising from peripheral nerve sheaths.
Schwannoma is a well-encapsulated solid lesion with non-aggressive slow-growth [1]. The bone lytic involvement is due to compression and not to schwannoma's inherent lytic properties. Long-standing schwannomas can show degenerative changes like cyst formation, haemorrhage and calcifications, which are not necessarily a sign of malignant evolution [2, 3]. Symptoms are caused by compression of the nerve itself or of adjacent structures.
Schwannomas can occur as single or, rarely, multiple lesions. While single schwannomas are sporadic, multiple schwannomas are generally associated with genetic disorders named neurofibromatosis, specifically type-2 neurofibromatosis and schwannomatosis. Schwannomatosis is a recently recognized distinct form of neurofibromatosis, characterised by the presence of two or more histologically-proved non-intradermal schwannomas in patients without type-2 neurofibromatosis. According to diagnostic criteria for definite schwannomatosis, brain MRI is required to exclude vestibular schwannomas [4]. After our patient underwent a brain MRI (not-shown), where neither vestibular schwannomas nor other lesions were found, the schwannomatosis diagnosis was confirmed.
A frequent feature of schwannomatosis is a segmental distribution of schwannomas. The multiple segmental schwannomas of our patient together with the location of the sacro-iliac lesion make this case particularly interesting. Sacral schwannomas are generally classified into: spinal dumbbell, retroperitoneal and intraosseous sacral schwannomas [2, 3]. To the best of our knowledge, no primary articular schwannoma of sacro-iliac joint has ever been described. So far, sacro-iliac joint involvement has been reported as following the extension of an intra-osseous sacral schwannoma [3].
Though a schwannoma diagnosis requires a histological examination, imaging is indispensable for the detection of clinically undetectable lesions and their local staging [1]. While non-contrast CT is mainly useful to assess bone involvement, which appears as osteolysis enclosed by sclerosis, MRI is the best modality for detecting lesions, assessing soft-tissue involvement and characterising heterogeneous schwannomas. On MRI lesions are iso-intense on T1-WI and iso- to hyper-intense on T2-WI [1, 4, 6]. DWI generally shows no diffusion restriction. Haemorrhagic components and calcifications appear as hypo-intense spots on T2* sequences and cystic or necrotic areas are typically hyper-intense on T2-WI. Schwanommas enhance vividly on post-contrast T1-WI. No imaging difference seems to exist between single sporadic schwannomas and multiple schwannomas in schwannomatosis [4].
Differential diagnosis of multiple non-infiltrative lesions includes neurofibroma and lymphoma. Giant cell tumour could be considered, especially in a peri-articular location, although it would typically be a single lesion, less hyper-intense on T2-WI and not surrounded by sclerosis [5].
Schwannoma of sacro-iliac joint in a segmental schwannomatosis.












Based on the CT and MRI images provided by the patient, the following main features are observed:
Based on the patient’s past medical history (previous surgery for a schwannoma in the right iliac region, multiple follow-ups thereafter) and the imaging features, the following differential diagnoses are considered:
Considering the patient's age, prior history of multiple schwannomas and post-surgical status, current imaging findings (multiple solid lesions located along peripheral nerve paths with bone lysis and a sclerotic rim), and the exclusion of acoustic neuroma meeting the diagnostic criteria for Schwannomatosis. Pathological examination also confirms a nerve sheath origin. Therefore, the most probable final diagnosis is:
Multiple Schwannomas (Schwannomatosis)
Surgical Treatment: For lesions causing significant symptoms (e.g., localized pain, nerve compression, functional impairment) or bony destruction affecting spinal stability, surgical resection or decompression is considered. For moderately sized lesions with slow growth and mild symptoms, treatment decisions can be tailored based on patient preference and a risk-benefit evaluation, including selective surgery or observation.
Conservative and Pharmacological Treatment: If lesions remain relatively stable and symptoms are manageable, regular follow-up and monitoring of lesion changes are recommended. For pain or mild functional impairment, the use of analgesics, nerve-modulating drugs (e.g., gabapentin), and physical therapy modalities can help relieve symptoms.
Other Interventions: In cases of potential nerve compression or higher risk of recurrence, an assessment of radiation therapy or newer treatments (such as stereotactic radiosurgery) may be considered. However, schwannomas are generally less sensitive to radiotherapy, so a combined assessment with surgical options is necessary.
Considering that the patient has undergone multiple surgeries, and that the affected areas include spinal and joint structures, rehabilitation exercise must be gradual and individualized.
Disclaimer: This report is a reference analysis based on the available imaging and clinical information. It does not replace in-person diagnosis or consultation by professional medical institutions. Specific treatment and rehabilitation plans should be tailored to the patient’s actual condition and confirmed by specialists and rehabilitation therapists.
Schwannoma of sacro-iliac joint in a segmental schwannomatosis.