Chronic shoulder instability secondary to glenoid dysplasia



Clinical History
A 25-year-old was referred to our radiology department complaining of left shoulder pain after repetitive shoulder dislocation secondary to hand support fall. He had also experienced a left acromioclavicular dislocation practicing sports 6 months before.
Imaging Findings
Shoulder arthrography was performed under fluoroscopic guidance using anterior approach and with gadolinium and iodine dilution injection, immediately the patient underwent CT arthrography (CTA) and MRI arthrography (MRA).
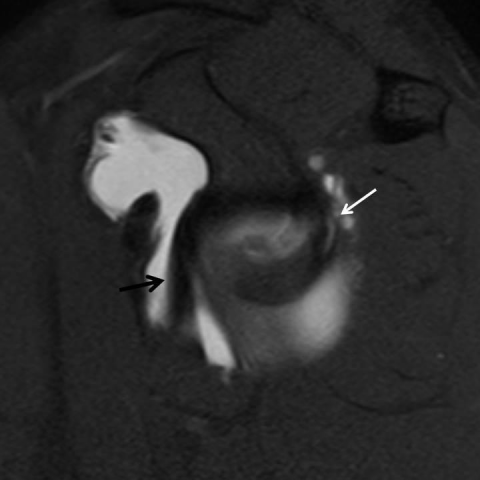
CTA and MRA showed a severe glenoid dysplasia with reduced volume of its posterior aspect and compensatory cartilage and labral hypertrophy. Buford complex with thickening of the middle glenohumeral ligament and hypoplasia of the anterosuperior labrum was also present. The anteroinferior labrum and the anterior band of the glenohumeral ligament were hypertrophic. Posterior labrum had a large tear extending from seven to twelve hours following the clockwise classification. The labral tear continued to the superior labrum, SLAP type 2 associated. A paralabral cyst was demonstrated with its origin depending on the type II SLAP lesion. A small chondral lesion was also shown.
Discussion
Glenoid dysplasia is a rare disorder defined as bone deficiency of the posteroinferior glenoid rim, with secondary hypertrophy of the adjacent cartilage [1]. It is more frequent than previously thought. Glenoid dysplasia has no sex predilection, it is frequently bilateral (60%), and its diagnosis can be made within a wide range of ages [2]. The pathogenesis appears to be a failure of ossification of the inferior cartilaginous glenoid and scapular neck. There are several associations described in the literature including multiple epiphyseal dysplasia, deficiencies of Vitamin C and D, muscular dystrophies, Erb’s palsy, haemophiliac arthropathy and neonatal septic arthritis. Familiar cases have also been reported [3]. Patients become symptomatic in their second or third decade of life, usually related to an increase in their daily or sport activity. There is a second peak described at the fifth or sixth decade [1]. Symptoms are pain, decreased range of movements and instability. Early osteoarthritis can be present [3]. Radiographic findings have been described on plain radiography, but CT and MRI have become the best techniques to study this abnormality, especially after intraarticular contrast injection [4]. Radiological findings are hypoplasia of the scapular neck and hypoplasia of the posterior glenoid with compensatory glenoid rim and labral hyperplasia. Hooking of the distal clavicle, enlargement of the coracoid process and acromion, and flattening of the humeral head can be present.
Glenoid dysplasia can be classified into mild, moderate and severe types. Especially moderate and severe types are frequently associated with posterior labral tears and posterior instability of the glenohumeral joint [1, 5]. We present the case of a 25-year-old man with left shoulder pain and instability. Severe glenoid dysplasia was demonstrated in CT arthrography and MR arthrography. In our patient extended posterior labral tear was present together with a SLAP type II lesion as described in the literature. In our case, there was hypoplasia of the scapular neck but no coracoid or humeral head alterations were seen.
Treatment is controversial, with most authors advocating conservative measures.
Differential Diagnosis List
Final Diagnosis
Severe glenoid dysplasia associated with posterior labral tear.
Liscense
Figures
Anteroposterior left shoulder radiography

CT arthrography

MR arthrography

MR arthrography
Glenoid dysplasia classification.

CT arthrography and MRI arthrography

Medical Imaging Analysis Report
1. Radiological Findings
From the patient's left shoulder X-ray, CT, and MR arthrography, the following findings are observed:
- Developmental dysplasia in the posteroinferior region of the scapular neck, with insufficient bony mass on the posteroinferior rim of the glenoid (consistent with severe glenoid dysplasia).
- CT arthrography shows proliferation of the posterior glenoid rim and posterior labrum with clear signs of tearing; MRI arthrography further confirms a wide-ranging posterior labral tear.
- A SLAP Type II lesion is observed on the same side (superior labral tear from anterior to posterior in the left glenohumeral joint), while the anterosuperior glenoid and humeral head remain basically normal, with no obvious hooked acromion or coracoid process abnormalities.
- No obvious humeral head flattening or dislocation is detected, suggesting that the main problems are located in the posteroinferior glenoid bone structure and the labrum.
2. Possible Diagnoses
- Glenoid Dysplasia: The patient’s posteroinferior glenoid bone defect and labral growth match typical imaging findings for this condition, and the patient is at a likely age for onset.
- Shoulder Instability (Posterior Instability): Due to posterior labral tear and bony deficiency, recurrent instability may occur, especially during repetitive shoulder abduction or weight-bearing movements.
- Shoulder Labral Tear (e.g., SLAP Lesion): Imaging has clearly identified a SLAP Type II tear, and other possible labral tears or combined injuries should be ruled out.
These listed possible diagnoses include both structural glenoid pathologies (congenital or developmental) and pathologies caused by shoulder instability and labral tears.
3. Final Diagnosis
Based on the patient’s medical history of recurrent left shoulder instability, as well as the X-ray and CT/MR arthrography findings of severe posteroinferior glenoid dysplasia, a significant posterior labral tear, and a SLAP Type II lesion, the most likely final diagnosis is:
“Severe Glenoid Dysplasia (with Posterior Labral Tear and SLAP Type II Lesion)”
4. Treatment Plan and Rehabilitation Program
Given that the patient’s main symptoms are instability and pain, the following conservative and surgical strategies are recommended:
- Conservative Treatment: Many studies suggest attempting conservative management first for cases of glenoid dysplasia with labral tears, including:
- Shoulder stability training: Strengthen the rotator cuff muscles (supraspinatus, infraspinatus, teres minor, and subscapularis) and the scapular stabilizers to improve dynamic joint stability.
- Use of a shoulder brace to avoid excessive abduction or external rotation, reducing the risk of recurrent dislocation.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) may be considered for pain and inflammation control.
- Surgical Treatment: If symptoms persist or repeated dislocations are severe, arthroscopic repair (labral repair, possible bone grafting, or stabilization procedure) might be necessary.
For rehabilitation and exercise prescription, follow the FITT-VP Principles (Frequency, Intensity, Time, Type, Progression):
- Early Rehabilitation Phase (Weeks 1-4):
- Frequency: 3-4 sessions per week.
- Intensity: Low-intensity isometric exercises, avoiding aggressive stretching of the posterior joint capsule.
- Time: 20-30 minutes per session, combined with brief cold therapy to reduce swelling.
- Type: Progress from passive to active range of motion exercises (e.g., gentle flexion-extension, internal-external rotation) along with activation exercises for the rotator cuff muscles.
- Progression: Gradually increase the range of motion and loading based on pain and mobility.
- Intermediate Strengthening Phase (Weeks 4-8):
- Frequency: 3-4 times per week, gradually increasing to 4-5 times.
- Intensity: Progress to moderate-intensity resistance exercises (e.g., resistance bands, lightweight dumbbells).
- Time: 30-45 minutes per session, incorporating both range-of-motion work and muscle strength exercises.
- Type: Moderate resistance training emphasizing coordination of the shoulder muscles, including comprehensive rotator cuff exercises (internal-external rotation, abduction, etc.).
- Progression: As shoulder stability improves, introduce core strengthening exercises and proprioceptive training.
- Late Sport/Activity Return Phase (Week 8 and Beyond):
- Frequency: 3-5 times per week, along with sport-specific training.
- Intensity: Progressively approach the intensity required for daily or sporting activities, but avoid repetitive loading in unstable positions.
- Time: 45-60 minutes per session, combining sport-specific practices with preventive exercises.
- Type: Gradual return to activities such as tennis or basketball; incorporate flexibility and scapular stability work.
- Progression: Reassess every two weeks based on functional recovery and adjust training methods and loads accordingly.
If there is significant bone fragility, poor overall fitness, or a high risk of recurrent dislocation, activity range should be further restricted and protective measures enhanced. Should conservative treatment be unsatisfactory, surgical intervention may be considered followed by personalized rehabilitation.
This report is a referential medical imaging analysis and should not replace in-person clinical evaluation or professional medical advice. Specific treatment plans should be determined after comprehensive assessment of the patient’s actual condition.
Human Doctor Final Diagnosis
Severe glenoid dysplasia associated with posterior labral tear.