Tenosynovial giant cell tumour localised type (L-TSGCT) of the ankle



Clinical History
A 38-year-old woman with a 2-year history of a slowly-growing mass on the anterolateral aspect of the left ankle. During that time the patient has reported minimal pain while walking or standing for prolonged periods, and the joint sometimes becomes inflamed when she overexerts.
Imaging Findings
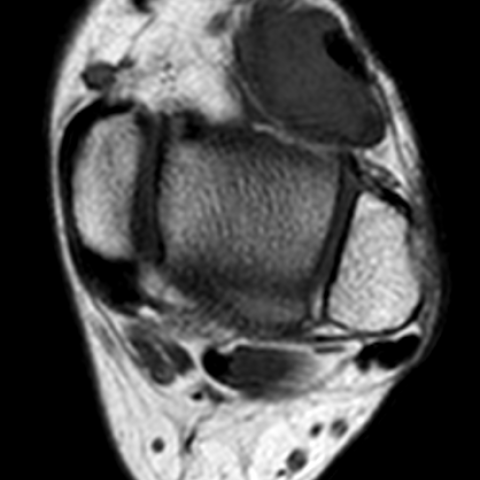
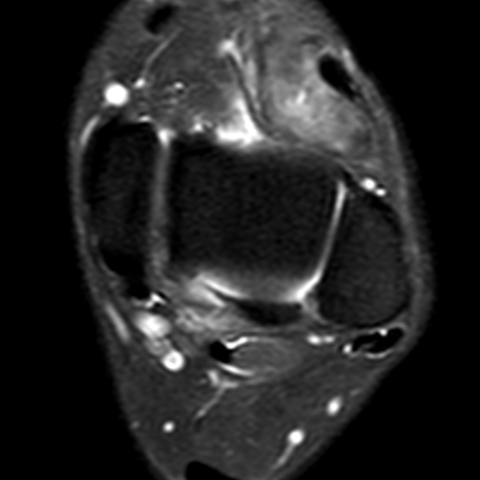
MRI was performed, demonstrating an oval and well-defined nodular lesion in the antero-lateral region of the ankle, in close relationship with the tendon sheath of the extensor digitorum longus. The image presents hypointense signal in T1 (Figures 1a, 1b and 1c) and intermediate signal in T2 sequences (Figure 2), with subtle areas of signal drop in sequences of magnetic susceptibility (Figure 3) and enhancement after administration of IV contrast (Figure 4).
The ultrasound evaluation showed a solid lesion, homogeneously hypoechoic (Figures 5a and 5b) with slight peripheral flow in the power Doppler study (Figure 6).
A US-guided biopsy was performed (Figure 7), and histopathological results were obtained (Figure 8).
Discussion
Background
Tenosynovial giant cell tumour (TSGCT) is the unifying term used in the 2020 WHO Soft Tissue and Bone Tumours Classification [1]. They have previously been known as pigmented villonodular tumours of the tendon sheath (PVNTS). It is a benign proliferative disease affecting synovial membranes, arising from the synovium of joint, bursae and/or tendon sheath. There are 2 forms, localised (L-TSGCT) and diffuse (D-TSGCT), which, although histologically similar, behave differently [3]. Localised tenosynovial GCT is more common, with a predominance for the hand and wrist, whereas the diffuse type is less common and affects the large joints (e.g., knee, hip, ankle) more [2]. It may be intra or extra-articular, and is classified as localised or diffuse, with diffuse forms being more aggressive. Extra-articular tenosynovial GCTs are most commonly periarticular in the lower limb (particularly the knee) but can be intramuscular or subcutaneous in location [1].
Clinical Perspective
TSGCT is a rare pathology affecting young subjects [4], mostly in the 4th and 5th decades of life [1]. The most frequent presentation is the localised form with a predilection for women. Localised forms predominate in the digits (85%), near the synovial sheaths or interphalangeal joints, more often on the palmar than the dorsal side and usually present as a single nodular lesion. Other less frequent locations comprise the wrist, foot and ankle, knee and, very rarely, hip or elbow [1,5]. Clinical presentation is relatively nonspecific [4].
Imaging Perspective
The gold standard for the diagnosis is MRI. Localised forms typically show a well-delineated lesion, in contact with the tendon sheath. Diffuse forms are usually articular.
The tendency of the lesions to bleed results in deposition of hemosiderin, more commonly in diffuse forms of the disease. The paramagnetic effect of hemosiderin results in the reduction of signal intensity in all pulse sequences, which is enhanced by highfield-strength and gradient-echo sequences. The reduction of signal intensity is more accentuated on T2-weighted images [6]. The signal is enhanced on gadolinium injection. Bone erosion and neurovascular encasement can be seen.
In ultrasound evaluation, most tumours are hypoechoic, homogeneous, posterior acoustic enhancement may be seen in some lesions, and typically show vascularity on power Doppler [7].
Outcome
The treatment of choice is surgery, and as TSGCT is most often present in the benign form, extensive surgery is generally not indicated. Localised forms usually permit total macroscopic resection and show little recurrence [8].
Teaching Points
TSGCT of the ankle is an uncommon localisation of the disease. Although the most frequent location is in the fingers, one should suspect it in other locations when the lesion is in close contact with synovial membranes. This is especially true when MRI shows a lesion with signal drop in magnetic susceptibility sequences.
All patient data have been completely anonymised throughout the entire manuscript and related files.
Differential Diagnosis List
Final Diagnosis
Tenosynovial giant cell tumour localised type (L-TSGCT)
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures









Imaging Findings
Based on the MRI and ultrasound images provided by the patient, there is a localized soft tissue mass in the anterolateral soft tissue of the left ankle joint. MRI shows that the mass is closely related to the tendon sheath, appearing as a relatively well-defined round/irregular lesion with uniform or slightly high signal on T1-weighted images and relatively low signal on T2-weighted images (suggesting potential hemosiderin deposition), with varying degrees of enhancement after contrast administration. No obvious joint surface destruction or significant bone erosion is seen; however, there is a mild compression effect on the adjacent soft tissue. On ultrasound, the lesion appears as a hypoechoic or relatively homogeneous echo, with a clear boundary and mild blood flow signal indicating abundant blood supply. Overall, the imaging findings are consistent with a benign lesion originating from the tendon sheath.
Possible Diagnoses
- Tenosynovial Giant Cell Tumor (TSGCT):
- Commonly found around the tendon sheath in the hand, but can also be seen around larger joints like the ankle and knee.
- MRI often shows hemosiderin deposition, appearing as low T2 signal with contrast enhancement.
- Consistent with the patient’s slow-growth pattern and relatively mild symptoms.
- Tendon Sheath Cyst or Synovial Cyst:
- Often located near joints or tendon attachments, generally showing high T2 signal due to fluid content.
- On ultrasound, they usually appear as anechoic or hypoechoic cystic structures.
- Other Soft Tissue Tumors (such as Schwannoma, Lipoma, Synovial Sarcoma, etc.):
- Must be considered based on lesion signal characteristics and clinical history. In atypical cases, biopsy is required to rule out rare malignant tumors.
Final Diagnosis
Considering the patient’s age, slow-growing clinical history, imaging features (especially the low T2 signal and enhancement on MRI), and the local lesion site, the most likely diagnosis is Localized Tenosynovial Giant Cell Tumor (TSGCT, focal type). If pathological results (if obtained) indicate the presence of macrophages, foam cells, and hemosiderin deposition, it can further confirm this diagnosis. If no pathological examination has been performed, surgical pathology confirmation is recommended.
Treatment and Rehabilitation Plan
Treatment Strategy:
Most cases are benign, and surgical resection is generally the first choice, with a low recurrence rate postoperatively. For localized TSGCT, complete excision under arthroscopy or open surgery is typically sufficient. If the lesion is relatively large or located near critical structures, thorough preoperative evaluation and planning are necessary.
Rehabilitation and Exercise Prescription:
- Early Postoperative Phase: It is recommended to immobilize or partially weight-bear on the ankle to protect it. During this period, gentle ankle movements (such as dorsiflexion and plantarflexion joint range-of-motion exercises) can be performed 2–3 times a day for 5–10 minutes each time, avoiding excessive loading and vigorous twisting.
- Intermediate Recovery Phase: Gradually increase weight-bearing and strength exercises, such as foot muscle training (toe flexion and extension, resisted ankle movements). Perform these 3–5 times per week for 15–20 minutes each session, adjusting dynamically based on pain and swelling.
- Late Functional Training Phase: If range of motion and muscle strength have recovered well, aerobic exercises (e.g., brisk walking, cycling) can be introduced at moderate intensity 3–4 times a week for about 30 minutes each session, combined with balance training (e.g., single-leg standing). During this stage, exercise intensity and duration should be increased gradually according to individual fitness, following the FITT-VP principle.
- Individualized Safety Considerations: If significant swelling or pain is noted at the surgical site, reduce or temporarily stop training and consult a physician. For those with underlying joint pathology or osteoporosis, progress should be more gradual, and external fixation or bracing may be used if necessary.
Disclaimer
This report serves only as a reference for medical analysis and cannot replace a professional physician’s consultation or formal treatment advice. Specific diagnoses and treatments must be based on the patient’s actual condition and the recommendations of a certified hospital and specialist.
Human Doctor Final Diagnosis
Tenosynovial giant cell tumour localised type (L-TSGCT)