Radiation-induced changes in the bone marrow



Clinical History
A 52-year-old female patient presented for the first follow-up 6 months after she had been treated for a mucoid liposarcoma anterior to the proximal medial tibia. The treatment included surgery and radiotherapy (50 Gy in 2 Gy fractions). The patient was asymptomatic.
Imaging Findings
MR imaging of the lower extremity at the site of previous operation and irradiation was performed. Multiple focal changes with intermediate signal on T1-w (Fig. 1), moderately increased signal on fluid sensitive sequence (Fig. 2) and moderate enhancement on fat-suppressed contrast enhanced T1-w images (Fig. 3) were disclosed.
Discussion
A. Radiation-induced changes in the bone marrow are very common and include fatty replacement, pathologic fractures, avascular necrosis, focal lesions of abnormal signal on MR imaging and rarely development of sarcoma [1, 2, 3]. Depending on the age of the patient and the amount of radiation, some changes may be reversible or not [4].
B. Clinical symptoms are usually absent with the exception of insufficiency fractures which occur in about 6% of cases [5]. The radiation-induced changes are mostly found during follow-up imaging. Careful attention should be paid to rule out the possibility of metastases.
C. MR imaging is the method of choice for assessing the bone marrow. During the first three days following irradiation (acute phase) the bone marrow undergoes excessive oedema which results in areas of reduced signal in T1-w and high signal on fluid sensitive MR images [4]. Between the third and the sixth week the bone marrow appears heterogeneous on T1-w MR images due to fatty replacement. After the sixth week, the lesions appear with high signal on T1-w images (in older patients), or with a region of central high signal and a peripheral intermediate one, due to haematopoietic regeneration (in younger patients) [6]. Many of those lesions may raise suspicion of recurrence. However, the absence of signs typical for metastatic deposits matched with the clinical picture of the patient, should help the radiologist to arrive at a final diagnosis of treatment-related changes. In inconclusive cases, a biopsy might be required, which, however, is invasive and may be complicated with fracture or infection [7]. In our case, the consecutive follow-up MR imaging studies up to 24 months after radiation showed no differences in the bone marrow changes suggesting the correct diagnosis.
D. No therapeutic procedure is needed. Nevertheless, follow-up MR imaging of the affected area must be required in inconclusive cases, in order to confirm their benign nature.
E. It is essential to recognize and differentiate post-radiation changes in the bone marrow from metastatic deposits in order to avoid unnecessary diagnostic tests and potentially harmful treatment.
Differential Diagnosis List
Final Diagnosis
Radiation-induced lesions of the bone marrow.
Liscense
Figures
T1-w MR image


Fat-suppressed PD-w MR image

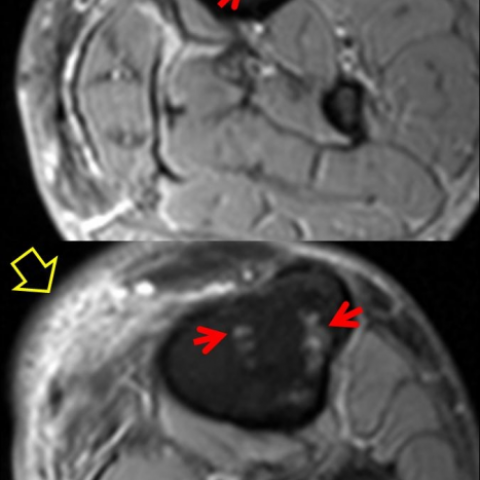
Contrast-enhanced fat-suppressed T1-w MR image


I. Radiological Findings
Based on the provided follow-up MRI images, multiple patchy and nodular signal changes are observed in the bone marrow of the medial proximal tibia in the surgical and radiotherapy region. Specifically:
- In the T1-weighted sequence, different degrees of decreased signal or high-signal patches are seen in the local bone marrow, suggesting fatty infiltration or regenerative changes.
- On T2 or fat suppression sequences, some regions exhibit high-signal intensity, indicating a certain degree of bone marrow edema or structural changes.
- Overall, there is no obvious cortical destruction, and no new abnormal mass or significant lesion is identified in the surrounding soft tissue.
- No obvious fracture lines or extensive bone destruction are observed, and the local soft tissue does not show abnormal enhancement indicative of tumor recurrence.
Overall, these bone marrow changes do not display typical neoplastic infiltration characteristics. They appear diffuse or patchy and are confined within the radiation field.
II. Differential Diagnoses
- Post-radiotherapy Bone Marrow Changes (Radiation-induced Bone Marrow Injury)
Reason: The patient previously received a 50 Gy dose of radiation therapy in this region. Common bone marrow reactions include fatty replacement, focal regeneration, or necrosis. On imaging, T1-weighted high signal or mixed signal changes may appear, and there are often no significant clinical symptoms. - Bone Metastasis or Tumor Recurrence
Reason: The patient was previously diagnosed with liposarcoma, so there is a risk of local or distant metastasis and recurrence. However, the current images do not show typical metastatic lesions (e.g., significant bone destruction or a soft tissue mass), and the patient also has no obvious clinical symptoms. - Radiation-induced Osteonecrosis or Early Pathological Fracture
Reason: Some patients may develop osteonecrosis or pathological fractures after a prolonged period following high-dose radiation. However, in this case, no obvious fracture line or sign of collapse is observed.
III. Final Diagnosis
Taking into account the patient’s age, past tumor history, local radiotherapy, and the extent and morphology of the bone marrow signal changes seen on the current MRI, alongside the lack of clinical symptoms, the most likely diagnosis is:
Post-radiotherapy bone marrow changes, with no clear evidence of tumor recurrence or bone metastasis.
It is recommended to have regular follow-up MRI examinations to further assess the stability of these bone marrow changes. If new clinical symptoms or suspicious imaging findings arise, a biopsy may be considered to confirm the diagnosis.
IV. Treatment Plan and Rehabilitation
Given that the imaging findings align with the clinical presentation, no specific treatment is needed at this time. The following management strategies may be considered:
- Continued Follow-up and Observation:
- Regular MRI follow-up (e.g., every 6–12 months) to evaluate changes in bone marrow signal and local bone structural stability.
- Monitor the patient closely; if pain, limited mobility, or other discomfort occurs, re-examination is recommended.
- Functional Exercise and Lifestyle Guidance:
- Recommend low-intensity, supported weight-bearing exercises such as moderate walking or using a stationary bike to maintain or improve lower limb function.
- Avoid excessive or high-impact activities (e.g., vigorous running and jumping) to reduce the risk of fracture.
- Example Exercise Prescription Based on the FITT-VP Principle:
- Frequency (F): 3–4 times per week.
- Intensity (I): Keep the heart rate at about 50–60% of the maximum heart rate (low to moderate intensity), ensuring no pain or significant fatigue.
- Time (T): 20–30 minutes per session, with the option to extend based on tolerance.
- Type (T): Choose exercises with less impact on the joints and bones, such as walking, swimming, stationary biking, or using an elliptical machine.
- Progression (P): Gradually increase exercise frequency up to 4–5 times per week or extend the duration by 5–10 minutes per session if well tolerated, avoiding abrupt increases in exercise volume.
- Individual Considerations:
- If the patient experiences mild local discomfort, consider using supportive devices or braces to reduce stress on the affected area.
- If significant pain or limited mobility occurs, high-load exercises should be discontinued, and the patient should seek medical advice promptly.
V. Disclaimer
This report is a medical analysis based on the current imaging and clinical information. It is for reference only and cannot replace a face-to-face consultation or the opinion of a professional physician. If the patient has any questions or changes in symptoms, they should promptly consult a specialist for further diagnostic and treatment advice.
Human Doctor Final Diagnosis
Radiation-induced lesions of the bone marrow.