Rheumatoid nodule of the foot - MRI features



Clinical History
A 56-year-old female patient presented with swelling and pain in the medial aspect of the left foot for the past month. No history of trauma or fever. She suffered from rheumatoid arthritis for several years on treatment.
Imaging Findings
A small nodular lesion showing T1W hypointense and T2W heterogeneously hyperintense signal was seen in the subcutaneous soft tissue along the medial aspect of the foot inferomedial to the first tasometatarsal joint. A central small cystic area was seen on T2W images. Mild surrounding oedema was noted. An area of focal inflammation with STIR hyperintense signal was noted in the heel pad inferior to the calcaneus, extending almost up to the skin. Multiple periarticular erosions were seen along the distal aspect of the lateral malleolus, calcaneus, talus, medial and intermediate cuneiforms. A valgus deformity of the forefoot was observed. The tendons appeared normal.
Discussion
Subcutaneous rheumatoid nodules are granulomatous nodules seen in 20% of patients with rheumatoid arthritis. They are frequently found on pressure points at bony prominences and extensor surfaces adjacent to joints, elbows, and fingers, as well as the forearm, metacarpophalangeal and proximal interphalangeal joints, occiput, back, heel, and other areas. Only 1% of cases occur in the foot, typically beneath the metatarsal head region. It is usually associated with seropositivity for rheumatoid factor [1].
The pathogenesis of rheumatoid nodules still remains unclear. Histologically, a rheumatoid nodule is composed of three zones: an inner zone of central necrosis, a middle cellular palisading area, and an outer granulomatous area with perivascular infiltration of chronic inflammatory cells [2].
They can also occur in patients with systemic lupus erythematosus, ankylosing spondylitis, granuloma annulare and chronic active hepatitis [1].
These are firm, nontender and moveable nodules ranging in size from 2 mm to 5 cm. Rarely they may ulcerate and can be painful [1].
The MR imaging characteristics of rheumatoid nodules are variable and non-specific. They appear most commonly as ill-defined nodular lesions isointense to muscle on T1W with heterogeneous intermediate to high signal on T2W. These nodules can appear solid showing homogeneous enhancement with contrast or cystic with peripheral rim enhancement. Sometimes a heterogeneous enhancement with central necrosis can also be seen [3, 4, 5].
The other hallmark findings of rheumatoid arthritis such as erosions and synovitis provides a clue to the diagnosis of these soft tissue nodules [6].
Ultrasound usually shows a homogenous hypoechoic lesion in the subcutaneous plane. A central discrete hypoechoic area may be seen in nodules with central necrosis [7]. USG done in our patient showed a well-defined hypoechoic lesion with a central hyperechoic area in the subcutaneous plane of the foot.
The common differentials include plantar fibromatosis, ganglion, tophus, cellulitis with abscess, proliferative fasciitis, lymphoma or sarcoma [3]. Plantar fibromatosis typically occurs along the plantar aponeurosis and shows hypo or isointense signal to skeletal muscle on both T1W and T2W images. Tophi usually show hypointense signal on T1W and intermediate signal on T2W images with other features of gouty arthritis.
Fine needle aspiration cytology done from the nodule in our patient revealed lymphocytes, neutrophils, histiocytes, few multinucleated giant cells and fibroblasts, in keeping with a chronic inflammatory pathology.
Differential Diagnosis List
Final Diagnosis
Rheumatoid nodule of the foot.
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Coronal T1W MRI image of the foot


Coronal STIR MR image


Sagittal STIR MR image

Sagittal T1W MR image

Cytology


USG of the foot



Coronal T1W and STIR MR image


Axial STIR and T2W MR image

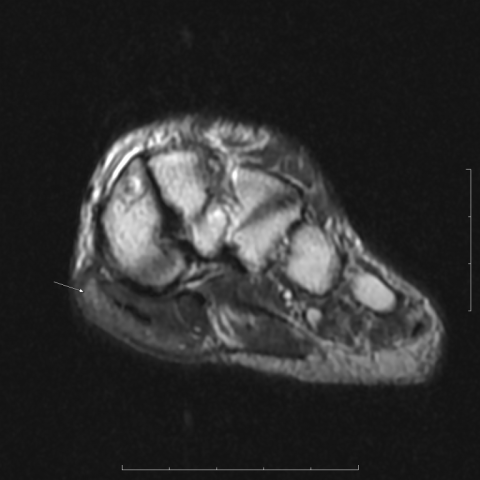
Axial T1W and STIR MR image


Axial T1W and STIR MR image


Imaging Findings
This case involves a 56-year-old female who presents with local swelling and pain on the medial side of the left foot for about one month. She has a past medical history of rheumatoid arthritis. Imaging examinations, including MRI and ultrasound, show the following:
- Ultrasound: A well-defined hypoechoic nodule is seen in the medial subcutaneous tissue of the foot, with areas of higher echogenicity within. This suggests possible central necrosis, fibrosis, or varied components inside the nodule.
- MRI (T1W, T2W, contrast-enhanced sequences): On T1-weighted imaging, the lesion mostly appears isointense or slightly hypointense relative to muscle. On T2-weighted imaging, it shows heterogeneous intermediate-to-high signal. Post-contrast images reveal peripheral or overall enhancement, with a possible central necrotic area. Mild soft tissue thickening is observed around the lesion, suggesting synovitis or local pressure changes. There is no obvious bone destruction, but there is mild thickening of the joint synovium consistent with chronic inflammation.
- The lesion is primarily located between the deep fascia and tendon in the subcutaneous layer, presenting as a nodular change with a relatively firm texture.
Potential Diagnoses
Considering the patient’s rheumatoid arthritis history and the imaging characteristics mentioned above, the following diagnoses or differentials should be considered:
- Rheumatoid nodule: Commonly found at sites of pressure or friction, such as the elbow, finger joints, and weight-bearing areas of the foot. On MRI, these nodules often appear as low to isointense signal on T1 and intermediate-to-high signal on T2, with possible ring or heterogeneous enhancement. Pathology or cytology may show granulomatous changes, central necrosis, and inflammatory cell infiltration.
- Tophus: Typically arises in joints or subcutaneous tissues, often accompanied by surrounding soft tissue inflammation. On MRI, tophi commonly display low signal on T1 and intermediate or mixed signal on T2, along with characteristic gouty joint changes. Clinically, they are often associated with hyperuricemia.
- Serous cyst / Ganglion cyst: Usually appears as a well-defined cystic lesion with more uniform fluid signal (high signal on T2, low on T1). Post-contrast images may show only a thin rim of mild enhancement.
- Tendon sheath tumor or other soft tissue tumors (such as synovial sarcoma, lymphoma, etc.): May present as a solid mass, often with more aggressive features or systemic symptoms.
Based on the imaging features (relatively clear border, potential central necrosis, and chronic inflammatory cell infiltration on histopathology) and the long-standing rheumatoid arthritis background, a rheumatoid nodule is the most likely diagnosis.
Final Diagnosis
Considering the patient’s age, gender, established rheumatoid arthritis history, and the ultrasound and MRI findings, together with cytological results (lymphocytes, macrophages, and granulomatous inflammatory cell clusters), the most probable diagnosis is:
Rheumatoid nodule.
Treatment Plan and Rehabilitation
For rheumatoid nodules, the specific treatment strategy depends on the severity of pain, functional limitation, and the activity of the lesion:
- Conservative management: In cases where the nodule is small and pain is not severe, controlling the underlying rheumatoid arthritis—such as adjusting DMARDs or using anti-inflammatory medications—may help. Avoid excessive pressure or friction on the affected area.
- Local injection: For nodules with significant redness or pain, a corticosteroid injection under sterile conditions may help reduce local inflammation. However, potential risks and side effects should be carefully evaluated.
- Surgical excision: For larger nodules that cause persistent pain or frequently ulcerate due to friction, surgical removal may be considered. The risk of surgery and the potential impact on local function should be weighed.
Rehabilitation/Exercise Prescription Recommendations:
- Principle: Gradual progression and individualization. Given the patient’s long-term rheumatoid arthritis, avoid excessive loading that may injure the joints. Emphasize gentle range-of-motion exercises and muscle strengthening.
- Early Phase: Low-intensity joint mobility
• Frequency: 1–2 times per day
• Intensity: Slight stretching and range-of-motion activities, primarily active joint movements
• Duration: 5–10 minutes each time, avoiding overexertion
• Methods: Gentle foot stretches and flexion-extension exercises of the metatarsophalangeal joints. These can be performed after a warm water soak or hot compress to reduce pain and stiffness. - Middle Phase: Enhancing joint stability and muscle strength
• Frequency: 3–4 times per week
• Intensity: Moderate resistance using bands or light strength training, avoiding sudden heavy loads
• Duration: 15–20 minutes each session
• Methods: Seated or standing heel raises and toe lifts, paired with low-impact aerobic exercises (e.g., cycling, swimming). - Late Phase: Functional weight-bearing and balance training
• Frequency: 3–5 times per week
• Intensity: Moderate intensity, gradually increasing based on patient tolerance
• Duration: 20–30 minutes each session
• Methods: Single-leg standing on a soft or balance pad to improve proprioception and posture correction. If foot pain subsides, gradually increase walking distance.
During exercise, be vigilant for significant increases in pain or swelling, or any other discomfort. If such symptoms occur, seek medical evaluation to adjust the training program.
Disclaimer: The above report is a reference analysis based on current information and does not replace an in-person consultation or the opinion of a professional physician. If you have any concerns or if your condition changes, please consult a specialist promptly.
Human Doctor Final Diagnosis
Rheumatoid nodule of the foot.