Extra-Abdominal Desmoid Tumor.



Clinical History
A 50 year-old-man presents with a 1-month history of a rapidly-growing left supraclavicular mass. On physical examination he presents hypoesthesia and dysesthesia of the medial face of the left arm. The patient does not refer weight loss or other symptoms.
Imaging Findings
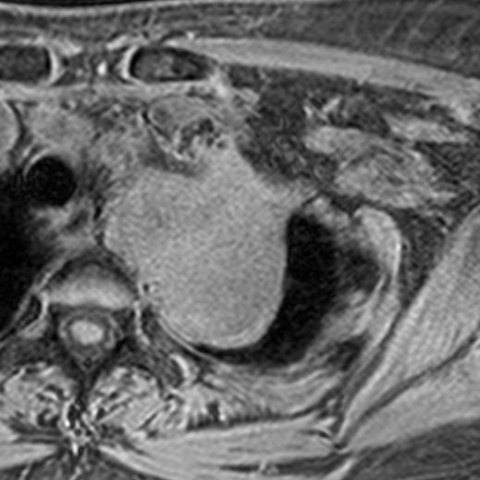
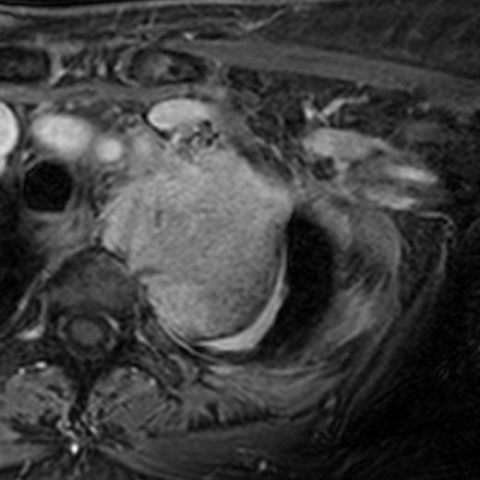
MRI was performed demonstrating a left low-cervical soft-tissue mass with low signal intensity in T1 and T2 weighted images, intermediate signal in STIR sequence and avid contrast enhancement in pre and post-contrast THRIVE imaging.
Axial images demonstrated focal areas of low intensity inside the lesion that in coronal images corresponded to very low intensity band-like images that crossed the lesion from cranial to caudal.
There is a minimum extension into the left conjunction foramen. The mass contacts with the right anterolateral border of the vertebral body, with a small focal area of cortical erosion.
A CT-guided biopsy was performed.
Discussion
A. Background:
Desmoid tumours (or deep fibromatoses) are a subset of fibroblastic of tumours of muscle, fascia or aponeurosis connective tissue. They present most commonly in adults between 25-35 years of age and are in some cases associated with Cr20 and Cr 8 trisomies [1].
B. Clinical Perspective:
They may be classified into intraabdominal, abdominal and extra-abdominal, depending on the localization of the tumour.
Intraabdominal desmoids may be mesenteric or pelvic. Mesenteric desmoids are associated (though not exclusive) to familial adenomatous polyposis (FAP or Garner syndrome) [1-4].
Abdominal desmoids affect the abdominal wall, predominantly abdominal rectus abdominis and obliquus abdominis muscles, and are affect mainly women either pregnant, in the first year postpartum or on oral contraceptive treatment [1, 2].
Extra-abdominal desmoids affect fasciae and muscles, and affect from most to least frequently: shoulder, thoracic wall, back, hip, and knee. They are very large tumours upon diagnosis (>5 cm), showing rapid growth and are very infiltrative. Desmoids are more aggressive the younger the patient, with a recurrence ratio of 87% in patients younger than 20-years-old, and around 20% in patients over 20-years-old [1].
C. Imaging Perspective:
MRI depicts best extra-abdominal desmoid tumours tissue and its relationship with surrounding structures. It demonstrates a large mass of infiltrative borders that expands along a fascial or muscular axis, often showing a "fascial tail" sign (80%) [1, 3, 5].
Signal is heterogeneous, varying with time depending on tissue composition. Early tumours have higher cellularity and tend to have a higher T2W signal, whilst tardy tumours have a more prominent collagen component and have a lower T2W signal [3-6]. Contrast enhancement tends to be moderate to intense [1, 3]. A typical sign of this type of tumour are longitudinal hypointense fibrous bands present in up to 86% ("black fingers") that correspond to fibrous bundles on pathological examination [1].
D. Outcome.
Management is surgical when possible, despite high recurrence rates. Radiation therapy is useful if this is not effective, also useful in recurrence prevention [2, 4-6].
E. Take home messages.
Extra-abdominal desmoids are very fast-growing infiltrative tumours with aggressive local behavior (not metastatic).
They tend to grow follow fascial and muscular planes, often identifying a "fascial tail".
They are of fibrous composition and usually have low signal in T1W and variable in T2W, with avid contrast enhancement.
Intratumoral fibrous bundles may be seen as lineal hypodense bands following the fascial or muscular axis.
Differential Diagnosis List
Final Diagnosis
Fibroblastic mesenchymal proliferation without cellular atypia: EXTRATHORACIC DESMOID TUMOR
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
MRI - STIR




MRI - Coronal THRIVE post-contrast


CT Guided Biopsy

MRI - Axial T1SE





MRI - Coronal T2WI




MRI - THRIVE pre and post-contrast enhancement
Medical Imaging Analysis Report
1. Radiological Findings
Based on the provided MRI images, a large mass is visible in the left supraclavicular region (deep to the trapezius and within the surrounding fascia and muscle layers), with unclear boundaries and evident infiltrative growth. On T1-weighted sequences, the lesion shows hypointense or isointense signals; on T2-weighted sequences, the signals are heterogeneous, with areas of relatively high signal interspersed with low signal. After contrast enhancement, the lesion parenchyma exhibits moderate-to-high enhancement. Imaging shows that the mass extends along the muscles and fascia, suggesting the presence of the “fascial tail sign.” Thin linear low-signal bands can be seen locally (possibly related to bundles of fibrous components).
Because the lesion is in the left supraclavicular fossa near the brachial plexus or neural pathways, it may correlate with the patient’s reported abnormal sensations (sensory loss and paresthesia) along the medial side of the left upper arm. No definitive evidence of distant metastatic lesions is currently observed.
2. Possible Diagnoses
-
Extra-abdominal Desmoid Tumor (also known as Deep Fibromatosis or Desmoid-type Fibromatosis)
Rationale: The tumor exhibits invasive growth within the fascia and muscle layers; MRI shows a typical infiltrative margin, relatively low T1 signal, and variable T2 signal; the lesion presents a “fascial tail sign” and thin low-signal areas (fibrous bundles). Clinically, these grow rapidly and rarely metastasize, consistent with deep fibromatosis. -
Soft Tissue Sarcoma (e.g., Fibrosarcoma or other sarcoma types)
Rationale: Soft tissue tumors, especially high-grade malignancies, can also present with rapid growth and invasive margins. However, deep fibromatosis tends to invade locally rather than metastasize, whereas some sarcomas often have a tendency to spread, thus differentiation is needed. -
Neurogenic Tumors (e.g., Schwannoma)
Rationale: Because the patient has symptoms of nerve involvement (abnormal sensation), a brachial plexus region tumor should be considered. However, neurogenic tumors usually have relatively well-defined margins on MRI, differ in enhancement patterns, and often do not exhibit the broad fascial infiltration seen in deep fibromatosis. -
Lymph Node Enlargement or Local Lymphoma Mass
Rationale: Supraclavicular lymph node enlargement is not uncommon clinically, but this lesion is large, exhibits marked myofascial infiltration, and its T2 signal pattern does not fully match typical lymph node enlargement or lymphoma, making this possibility relatively less likely.
3. Final Diagnosis
Taking into account the patient’s status as a middle-aged male, rapid tumor growth, location in the shoulder girdle and adjacent fascial tissues, as well as the characteristic MRI features (“fascial tail sign,” low/isointense T1 signal, variable T2 signal, and marked enhancement) and the clinical history, the most likely diagnosis is an extra-abdominal desmoid tumor (deep fibromatosis) in the shoulder (supraclavicular fossa) region.
If histologically confirmed, it can be definitively identified as a deep fibromatosis. If pathological evidence remains insufficient, a biopsy or surgical resection for pathological examination is recommended for a final diagnosis.
4. Treatment Plan and Rehabilitation
4.1 Treatment Strategy
- Surgical Treatment: If a deep fibromatosis can be completely resected without causing severe functional impairment, surgery is the first choice. However, these tumors have a certain recurrence rate, and complete excision with preservation of vital neurovascular bundles is crucial.
- Radiation Therapy: For cases where complete resection is not feasible, or in the event of positive surgical margins or a high risk of local recurrence, radiation therapy can be considered as an adjunct or definitive treatment.
- Pharmacotherapy: Some patients may attempt conservative treatment with steroids, anti-estrogen medications (e.g., tamoxifen), or NSAIDs. However, efficacy varies among individuals.
- Chemotherapy: Usually reserved for inoperable, recurrent, or persistent cases, administered on a case-by-case basis.
4.2 Rehabilitation and Exercise Prescription
After completing treatment (whether surgical, radiation, or otherwise), individualized rehabilitation is needed to restore function of the affected shoulder, neck, and upper limb. Below are general guidelines based on the FITT-VP principle (frequency, intensity, time, type, and progression):
- Early Postoperative (or Post-Treatment) Phase:
- Frequency: 1-2 times per day, short sessions with gentle movements.
- Intensity: Low intensity; perform passive or assisted activities without inducing significant pain.
- Time: About 10-15 minutes per session.
- Type: Active/passive range-of-motion exercises for the shoulder, neck, and upper limb joints (e.g., shoulder flexion, abduction, gentle internal and external rotation), combined with simple finger and wrist movements.
- Intermediate Recovery Phase:
- Frequency: 3-4 days per week.
- Intensity: Increase resistance gradually (e.g., light resistance bands or paddle exercises) in the absence of significant pain or swelling. Avoid overloading the neck and shoulder.
- Time: 20-30 minutes per session.
- Type: Strengthening exercises for the shoulder girdle musculature and core stabilization (e.g., side plank, supine bridge) to improve overall support. Ensure proper posture and avoid improper force application that could cause strain.
- Late Consolidation Phase:
- Frequency: 3-5 days per week.
- Intensity: Progress to moderate-intensity exercises with controllable discomfort, such as using small dumbbells to train the shoulder and neck muscles.
- Time: 30-45 minutes per session, adjusted according to tolerance.
- Type: Incorporate aerobic activities (e.g., brisk walking, cycling) alternated with strength training to enhance cardiorespiratory function and maintain muscular strength and flexibility.
If the patient has osteoporosis, compromised cardiopulmonary function, or other comorbidities, exercise intensity and volume should be adjusted under professional supervision to ensure safety.
Disclaimer: This report is a reference medical analysis based on the available information and does not substitute for an in-person consultation or professional medical advice. If you have any questions, you should promptly consult a qualified physician or seek further evaluation and treatment at a reputable medical institution.
Human Doctor Final Diagnosis
Fibroblastic mesenchymal proliferation without cellular atypia: EXTRATHORACIC DESMOID TUMOR