Quadriceps fat pad syndrome



Clinical History
33-year-old male patient who had a one year history of recurrent anterior knee pain, more severe on prolonged sitting. No history of recent trauma.
Imaging Findings
PD fat-suppressed sagittal MR images of the knee show extensive quadriceps fat pad oedema with intact extensor mechanism. The rest of the knee joint was normal without evidence of bone, ligament or meniscal injury or pathology.
Discussion
Anterior knee pain, the most common knee complaint, may be caused by a variety of abnormalities that include cartilage disease, patellar instability/dislocation, femoral trochlear dysplasia, tendinopathies, bursal conditions, mediopatellar plica syndrome and Hoffa’s disease. It is not difficult to diagnose these on MRI, although less common aetiologies may be overlooked in spite of the patient’s significant complaints [1-5].
There are three normal fat pads located about the anterior knee: quadriceps (anterior suprapatellar), prefemoral (posterior suprapatellar), and Hoffa (infrapatellar) fat pads. Each is interposed between the joint capsule externally and the synovium-lined joint cavity, making it intracapsular but extrasynovial [6]. Previous studies have demonstrated abnormal MR appearance of these fat pads in relation to symptomatic knees without evidence of internal derangement [4, 6-8].
A normal quadriceps fat pad lies on the patellar base and is triangular, filling the gap between the posterior aspect of the quadriceps tendon insertion and the superior aspect of the retropatellar cartilage to increase the congruency of the extensor mechanism [7, 8]. Focal inflammation involving the anterior suprapatellar fat has been described, manifested on MRI as low T1/high T2 signal with accompanying mass effect on the quadriceps tendon and suprapatellar recesses [8]. Additionally, some have described its imaging appearance as resembling that of Hoffa disease but in a different location [6, 7]. Proposed aetiologies include developmental changes in the anatomy of the extensor mechanism, abnormal mechanics [8], chronic microtrauma or overuse injury [6]. Although some authors favour the overuse mechanism based on its imaging similarities to Hoffa disease, young male predominance, lack of significant association with patellofemoral malalignment or osteoarthritis and symptomatic involvement in highly active patients [6], other more recent investigations have theorized that fat pad oedema may be an early manifestation of an inflammatory process such as rheumatoid arthritis [9, 10].
Because the exact cause of quadriceps fat pad enlargement associated with anterior knee pain at physical examination is not known, a treatment for this problem is also not known. Roth et al. used conservative measures such as physical therapy and intraarticular corticosteroid injection with eventual symptomatic improvement [8]. No surgical management has been reported in existing literature.
Quadriceps fat pad syndrome is a diagnosis of exclusion which must be considered in a highly active patient with persistent anterior knee pain and without evidence of trauma or internal joint derangement. Alternatively, it may also herald the presence of a more systemic inflammatory process such as rheumatoid arthritis.
Differential Diagnosis List
Final Diagnosis
Quadriceps fat pad syndrome
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Schematic diagram of the normal fat pads of the knee
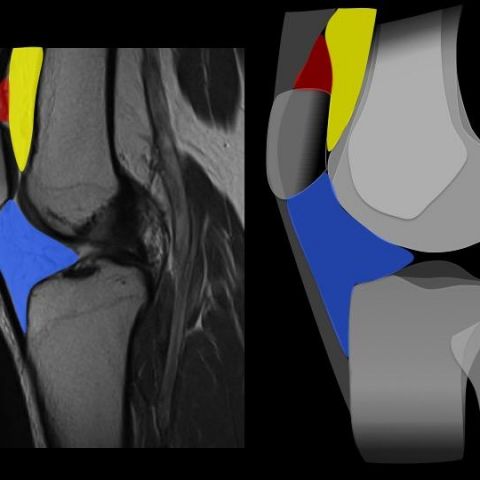
Sagittal MR image and diagram of the quadriceps fat pad

Sagittal and axial MR images of the quadriceps fat pad

Knee Joint Imaging Analysis Report
I. Imaging Findings
Based on MRI sequences, a significant abnormal signal change was noted in the fat pad of the anterior region of the patient’s right (or left) knee joint (above the quadriceps tendon insertion):
- On T1-weighted images, the fat pad area appears as relatively low signal.
- On T2-weighted images and fat suppression sequences, the area shows high signal, suggesting edema or inflammatory changes.
- Mild local swelling is observed, indicating slight compressive/mass effect on the quadriceps tendon and the joint capsule.
- No clear signs of intra-articular structural damage (e.g., meniscal tear, ligament rupture) or extensive cartilage wear are detected.
Clinically, the patient presents with persistent anterior knee pain, aggravated by prolonged sitting or flexed knee positions, which is consistent with the MRI findings of fat pad edema. There is no significant history of acute trauma, and acute fracture or soft tissue tear has been ruled out.
II. Potential Diagnoses
- Quadriceps Fat Pad Syndrome
This syndrome can lead to anterior knee pain, and imaging often reveals fat pad edema signals (T2 hyperintensity). Symptoms related to activity and posture may be detected during physical examination. Patients are often young and physically active. - Chondromalacia Patella
Commonly found in patients with anterior knee pain, usually showing cartilage thinning or abnormal subchondral bone signals. In this case, no significant cartilage structural damage is observed, making this diagnosis less likely. - Patellar Tendinitis or Other Tendinopathies
These can also cause anterior knee pain, often accompanied by high signal changes around the patellar tendon or quadriceps tendon on imaging. However, this case primarily involves the quadriceps fat pad, which does not fully match the typical location of patellar tendinitis. - Other Inflammatory Intra-Articular Changes (e.g. Early Rheumatoid Arthritis)
If there is a widespread joint inflammatory response, the fat pad may be involved. Currently, the primary finding is localized fat pad edema without obvious synovitis or articular surface erosion, so this possibility remains to be excluded.
III. Final Diagnosis
Considering the patient’s age, clinical presentation (anterior knee pain aggravated by prolonged sitting or knee flexion), and imaging findings (T2 hyperintensity and slight swelling of the quadriceps fat pad without significant intra-articular structural damage), the most likely diagnosis is “Quadriceps Fat Pad Syndrome.”
If clinical symptoms persist or if laboratory markers such as rheumatoid factor or inflammatory indicators become abnormally elevated, further evaluation is advised to rule out early inflammatory joint diseases.
IV. Treatment and Rehabilitation Plan
1. Conservative Treatment
- Use non-steroidal anti-inflammatory drugs (NSAIDs) or intra-articular/local corticosteroid injections to reduce inflammation and pain.
- Employ physical therapy for anterior knee pain, such as ultrasound therapy, hot/cold compresses, and muscle relaxation exercises.
- Temporarily reduce or avoid movements or postures that provoke pain (e.g., deep squats, prolonged sitting with knee flexion) to minimize irritation.
- Where possible, use knee braces or patellofemoral offloading devices to relieve pressure on the anterior knee structures.
2. Physical Rehabilitation and Exercise Prescription (FITT-VP Principle)
After pain subsides and inflammation decreases, a gradual knee function and muscle strength training program can be initiated to help stabilize the patellofemoral joint and reduce recurrence. An example outline is as follows:
- Frequency (F): 3–4 times per week, ensuring no significant knee pain or swelling.
- Intensity (I): Start with low intensity, avoiding deep knee flexion exercises (e.g., seated leg raises, isometric quadriceps contractions with a resistance band). Once pain improves, progressively increase the range of motion.
- Time (T): About 20–30 minutes per session, adjusted based on individual tolerance.
- Type (T):
• Early Phase: Active range-of-motion exercises, static quadriceps contractions.
• Intermediate Phase: Gradually introduce seated straight leg raises, low-load squats (shallow squats), step exercises.
• Late Phase: Add resistance band training, low-impact aerobic exercises (fast walking, rowing machine, etc.) to enhance muscle strength and joint stability. - Progression (P): Gradually increase load or movement range, provided there is no significant discomfort, in order to promote recovery of muscle and joint function.
If any marked pain or discomfort appears during training, re-evaluation and reduction of training intensity is recommended in a timely manner. Consult with rehabilitation or sports medicine professionals if necessary to develop an individualized program.
3. Surgical Treatment
Currently, there are no well-established surgical indications for Quadriceps Fat Pad Syndrome in the literature. If a patient does not respond well to conservative treatments or injections and demonstrates significant structural changes, discussion with an orthopedic surgeon regarding possible, though rare, surgical interventions may be warranted.
Disclaimer: This report is for clinical reference only and does not replace in-person consultations or other professional medical advice. If you have questions or if your condition changes, please seek professional medical evaluation and treatment promptly.
Human Doctor Final Diagnosis
Quadriceps fat pad syndrome