Anterior cruciate ligament avulsion fracture



Clinical History
12-year-old boy who fell on his knee.
Companion Case: 21 F with limited knee extension 5 months after accident.
Imaging Findings
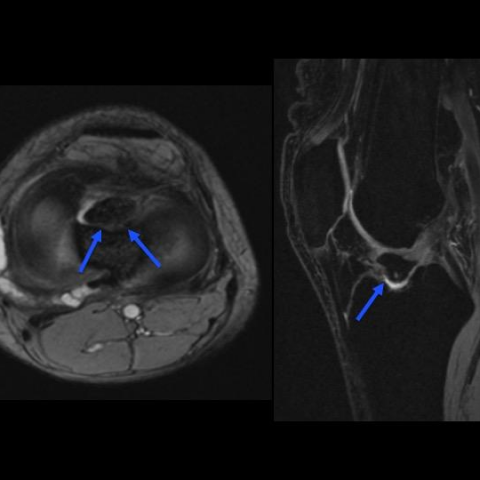
(Fig. 1-2) Coronal and sagittal MR images of the knee showing a recent, minimally displaced anterior tibial spine fracture fragment attached to an intact anterior cruciate ligament (ACL).
(Fig. 3-6) Companion case of a 21-year-old female patient with plain radiographs and MR images demonstrating a remote nonunited tibial fragment attached to an intact anterior cruciate ligament.
Discussion
The anterior cruciate ligament attaches proximally to the posterior medial surface of the lateral femoral condyle and distally to the anterior intercondylar area in the tibia. Its tibial insertion is broad and fanlike and is located slightly lateral and anterior to the anterior tibial spine [1]. Although tearing of the anterior cruciate ligament most commonly occurs at its midsubstance, an avulsion fracture of the ligament from its tibial insertion occurs in a minority of cases and is more common in children than in adults, particularly those between eight to thirteen years of age [1-2]. These injuries are more common in the skeletally immature population due to the relative increased strength of the ligament compared with the developing bone and growth plate [3]. In children, this injury occurs secondary to hyperflexion of the joint and internal tibial rotation and is uncommonly accompanied by other ligamentous injuries [1-2].
On conventional radiographs, these avulsion fractures may be difficult to recognize, although the presence of a small bone fragment in the region of the intercondylar notch with cortical irregularity of the adjacent tibial eminence suggestive of a donor site may be the usual findings. MR imaging is useful for confirmation of the tibial site of the fragment, evaluation of the rest of the ligament and assessment for additional injuries [2].
It is crucial for the radiologist to accurately identify this injury. Failure or delay in diagnosis may eventually result in nonunion and persistent clinical symptoms such as limitation or pain on knee extension and anterior instability [4]. In addition, classification of ACL avulsion fractures may dictate the management. The Meyers and McKeever classification system describes four subtypes of tibial spine fractures: presence of a minimally displaced fragment (type I), anterior elevation of the fragment (type II) complete separation of the fragment from the tibia (types III and IV) with rotational component or comminution (type IV). Type I injuries are managed conservatively, while arthroscopy is recommended for type II– IV lesions with types III and IV injuries requiring internal fixation [5].
In conclusion, it is imperative for the radiologist to recognize and correctly diagnose an ACL avulsion fracture to facilitate early and appropriate management and prevent future anterior knee instability.
Differential Diagnosis List
Final Diagnosis
Anterior cruciate ligament avulsion fracture
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Coronal MR images of the knee

Sagittal MR images of the knee

Companion Case: 21 F with limited knee extension 5 mos. after accident

Companion Case: 21 F with limited knee extension 5 months after accident

Companion Case: 21 F with limited knee extension 5 months after accident
Companion Case: 21 F with limited knee extension 5 mos. after accident

Medical Imaging Analysis Report
I. Imaging Findings
- On the anteroposterior and lateral X-rays of the knee joint, an abnormal small bone fragment can be observed in the intercondylar eminence (tibial spine) region of the tibia, suggesting cortical discontinuity or the presence of fracture fragments in that area.
- MRI shows abnormal signal at the tibial attachment of the anterior cruciate ligament (ACL), with some ligament fibers connected to the fracture fragment; localized bone marrow edema is noted at the tibial spine.
- No significant extensive tearing is observed in the surrounding soft tissues. A small amount of effusion is present in the joint cavity, and the cartilage surface appears generally intact.
- No obvious signs of rupture or significant injury are noted in other ligaments (e.g., posterior cruciate ligament, medial or lateral collateral ligaments).
II. Potential Diagnoses
- ACL Avulsion Fracture at the Tibial Attachment
- The patient’s age and mechanism of injury (falling trauma to the knee) match the common population (8–13 years old) for this type of fracture.
- X-ray shows a small bone fragment at the attachment site, and MRI further demonstrates the connection between the ligament and the bone fragment, along with bone marrow edema at the tibial spine.
- Simple Tibial Spine Fracture
- This is a selective fracture involving the tibial spine, which may not necessarily be associated with avulsion of the ACL. A careful assessment of ligament integrity is required; however, in this case, MRI evidence of ligament signal changes makes this less likely.
- Partial ACL Strain or Tear
- If it were purely a ligament injury, MRI would show partial interruption of ligament continuity or abnormal signal, but there would be no obvious bone fragment displacement.
III. Final Diagnosis
Based on the patient’s age of 12 years, history of trauma from a fall, and imaging findings, the most likely diagnosis is “ACL Avulsion Fracture at the Tibial Attachment.” This injury is relatively common in children and is associated with hyperflexion and internal rotation stress.
IV. Treatment Plan and Rehabilitation
According to the Meyers and McKeever classification, if the fracture fragment displacement is minor (Type I or II), conservative treatment may be considered; if the displacement is significant (Type III or IV), arthroscopic surgery or internal fixation is required to stabilize the fragment and protect ligament function.
- Conservative Treatment (for minimally displaced or stable fractures)
- Use a cast or brace to keep the knee joint in an appropriate degree of flexion for several weeks, followed by a gradual increase in activity.
- Avoid weight-bearing and excessive flexion-extension movements in the early stage to reduce the risk of secondary injury.
- Surgical Treatment (for significantly displaced or unstable fractures)
- Arthroscopic reduction with internal fixation (e.g., screws or suture fixation) to ensure stable healing of the fracture fragment at the ligament attachment site.
- Postoperatively, a brace is required, followed by a stepwise rehabilitation training program.
Rehabilitation/Exercise Prescription Suggestions (FITT-VP Principle)
The following rehabilitation training program should be carried out under the guidance of a specialist or physical therapist, and adjusted flexibly according to the patient’s individual recovery status:
- Frequency: In the early stage, 1–2 sessions of light exercise per day, and as knee function improves, increase to 3–5 times per week.
- Intensity: Begin with an intensity that does not cause significant pain or discomfort; as range of motion and muscle strength improve, progressively increase resistance training (e.g., choosing higher tension bands).
- Time: Initially limit each session to 10–15 minutes, gradually extending to 30 minutes or more.
- Type: Recommended phases include:
- Early Stage: Quadriceps isometric contractions, straight leg raises, and non-weight-bearing range of motion exercises.
- Intermediate Stage: Gradually introduce partial weight-bearing exercises (e.g., walking with crutches), balance training, and light strength exercises.
- Late Stage: Jogging, shallow squats, lower extremity proprioception training, etc.
- Progression: Based on pain, swelling, and joint stability; gradually increase the difficulty and load of the training.
If bone fragility or other medical conditions (e.g., poor cardiopulmonary function) are present, further reduction of training volume or shorter sessions may be needed, and close monitoring of the patient’s condition is necessary.
Disclaimer: This report is based on available imaging and medical history for reference purposes and does not replace face-to-face consultation or professional medical advice. If you have any questions or if symptoms worsen, please contact a specialist doctor or return to the hospital for follow-up treatment.
Human Doctor Final Diagnosis
Anterior cruciate ligament avulsion fracture