Unusual cause of low back pain: Osteosarcoma of the iliac bone



Clinical History
A 29-year-old man presents at the radiology department complaining of low back pain since 4 months, not radiating to the leg. There was no history of trauma.
Imaging Findings
Digital radiography revealed increased density of the left iliac wing (Figure 1).
Computer Tomography (CT) was performed in the same week of the radiograph, confirming sclerosis of the left iliac bone. A sunburst periosteal reaction and osteoid matrix formation in the adjacent soft tissue were seen with extension into the sacroiliac joint (SIJ) (Figure 2).
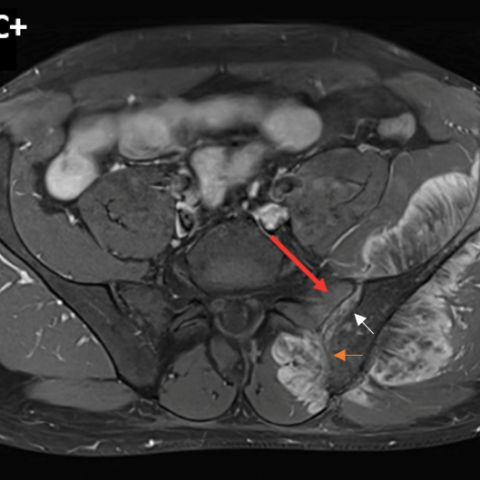
On Magnetic Resonance Imaging (MRI), the bone marrow of the left ileum was hypo-intense on T1- and T2-weighted images (WI). A large heterogeneous soft tissue component was seen on fat-suppressed (FS) T2-WI, FS T1-WI and T1-WI without FS. Diffusion-weighted imaging (DWI) showed diffusion restriction at the periphery of the lesion. After administration of gadolinium contrast, there was enhancement of the non-mineralised component. Transarticular involvement of the SIJ was seen (Figures 3a, 3b, 3c, 3d and 3e). Neo-adjuvant chemotherapy was started, followed by surgical hemi-pelvectomy and partial resection of the sacrum.
Histopathology confirmed the imaging diagnosis of osteosarcoma.
Discussion
Osteosarcoma (OS) is the most common primary bone tumour in adolescents, with a slight male predominance. Osteoid matrix formation is characteristic. OS typically occurs in the metaphysis of the long bones, with the knee being the most frequent localisation. Epiphyseal extension and joint involvement are common [1].
Primary involvement of the iliac bone is less common. Tumours located next to the SIJ need a precise evaluation with respect to their relationship to the joint, as this has a significant implication on surgical management. As a general rule, the synovial part of the joint constitutes a barrier, and extension will preferably occur through the ligamentous part of the joint [2]. However, aggressive tumours such as OS will occasionally extend through the synovium.
Non-specific pain and local swelling are usually the first signs of OS. Pathological fractures may also occur.
Radiography is the initial imaging modality of choice. Usually, the osteoid matrix production is sufficient to result in a cloudy moth-eaten area of increased density. Cortical destruction, with often extension into the soft tissues and aggressive periosteal reactions such as Codman triangle, onion skin and sunburst, is readily seen in long bones on radiographs but is far less evident in areas with a complex anatomy and superimposition such as the axial skeleton [1]. CT may play an additional role in detection and characterisation on these locations.
MRI is pivotal in local staging, evaluation of soft tissue extension and articular involvement. T1-WI is the most accurate sequence for the evaluation of tumour extension, which is often overestimated on T2-WI [3]. The osteoid matrix is of low signal on both T1- and T2-WI. DWI complements conventional T1- and T2-weighted imaging by early detection, adequate assessment of tumour extension and follow-up after therapy. Solid components enhance after administration of gadolinium contrast.
Histopathology is required for the final diagnosis. Different histological subtypes are identified depending on the dominant matrix. Sometimes the osteoid matrix is very subtle or cannot be seen macroscopically, which can make differential diagnosis very difficult [2,4].
The differential diagnosis with Ewing sarcoma is important, as it is more common in the pelvis than osteosarcoma. Ewing sarcoma usually presents with a larger soft tissue component and lacks osteoid matrix, although reactive bone formation is possible, which can make histological differentiation challenging [4].
Treatment consists of surgical resection and chemotherapy. Neo-adjuvant therapy is initiated for tumour volume reduction prior to surgery if limb-sparing approach is feasible [3].
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Osteosarcoma
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Radiograph of the pelvis

CT of the pelvis

MRI of the pelvis




1. Imaging Findings
Based on the provided X-ray, CT, and MRI images, a lesion is identified in the right iliac region, with the following characteristics:
- On the pelvic AP X-ray: A high-density area (indicated by the arrow) is visible in the right iliac bone, showing an irregular “cloud-like” appearance and signs of cortical destruction.
- CT axial view: Local bone destruction within the right iliac bone, accompanied by uneven sclerosis and a soft tissue mass. Some areas exhibit a “moth-eaten” appearance; there is extension into the iliacus region and the pelvic cavity. Lesion involvement near the sacroiliac joint (SIJ) is visible, raising concern for joint space invasion.
- On MRI sequences: The lesion shows intermediate to low signal intensity on T1-weighted images and heterogeneous signal intensity on T2-weighted images. Low-signal strip-like components within the tumor suggest osteoid matrix (osseous or calcified components). The solid portion of the tumor demonstrates significant enhancement on contrast scans and appears hyperintense on diffusion-weighted imaging (DWI), indicating areas of high cellular density.
- No obvious pathologic fracture is noted, but there are signs of soft tissue involvement, suggesting the possibility of early or micro-fractures.
2. Potential Diagnosis
Considering the patient’s age (29 years old), symptoms (persistent lower back pain for 4 months, no significant history of trauma), and imaging findings, possible diagnoses and differential diagnoses include:
- Osteosarcoma: Most frequently occurs in adolescents and young adults. It can present with osteoid matrix formation, bone destruction, and a concurrent soft tissue mass. On imaging, it often appears as a “cloud-like” or irregular enhancing lesion.
- Ewing Sarcoma: Commonly found in the pelvis and other locations, often presenting as a more homogeneous soft tissue mass. It typically lacks prominent osteoid matrix, although reactive new bone formation can occasionally occur, necessitating differentiation from osteosarcoma.
- Other malignant tumors or metastases: This includes other primary bone tumors or metastases from other origins. Differentiation is typically based on the patient’s history, imaging features, and pathological examination.
3. Final Diagnosis
Based on imaging findings (osteoid matrix formation, bone destruction, and soft tissue involvement) and the patient’s pathological examination results, the most likely final diagnosis for this lesion is:
Osteosarcoma.
If pathological confirmation has not yet been obtained, a further biopsy or consultation with a bone tumor specialist is recommended to establish a definitive diagnosis.
4. Treatment Plan and Rehabilitation
The primary treatment options for osteosarcoma include:
- Surgical Resection: For lesions amenable to local resection, a wide excision (ensuring negative surgical margins) is recommended. For pelvic involvement, it is necessary to evaluate the extent of sacroiliac joint involvement to determine the appropriate surgical approach.
- Chemotherapy: Neoadjuvant chemotherapy (preoperative chemotherapy) is routinely used to shrink the tumor and improve the likelihood of limb- or function-sparing surgery. Adjuvant chemotherapy (postoperative) is also administered to reduce the risk of recurrence and metastasis.
- Radiotherapy: In specific circumstances, radiotherapy may be considered as an adjunct. However, osteosarcoma has limited radiosensitivity; radiotherapy is usually reserved for cases not suitable for complete surgical excision or patients who cannot tolerate major surgery.
Rehabilitation/Exercise Prescription Recommendations:
- Plan rehabilitation according to the surgical and chemotherapy protocols. Preoperative exercises may include light muscle strengthening, such as core training and hip joint stabilization, avoiding excessive loading.
- Early Postoperative Phase (first 4-6 weeks): Focus on protecting the surgical site and maintaining joint range of motion. Begin with passive joint mobilization or low-load assisted exercises. If surgery involves the lower extremities or the pelvic region, assistive devices (e.g., walker) may be used to minimize weight-bearing.
- Intermediate Rehabilitation (6-12 weeks): Once bone healing has sufficiently progressed, gradually transition to active joint mobility exercises, low-intensity resistance training, and low-impact aerobic workouts such as swimming or stationary cycling.
- Late Rehabilitation (12 weeks and beyond): Gradually increase resistance training intensity and extend aerobic exercise duration. Follow the FITT-VP principles (Frequency, Intensity, Time, Type, Progression, and Individualization). If tolerated, progressively reintroduce higher weight-bearing functional training.
- Throughout the entire rehabilitation process, closely monitor pain, local swelling, and overall condition (e.g., body temperature, blood counts). Communicate promptly with the attending physician and rehabilitation therapist if any concerns arise.
Disclaimer
This report is based solely on the provided images and related information for academic and reference purposes and is not a substitute for in-person consultation or the medical advice of a licensed physician. If you have any questions or changes in your condition, please seek professional medical services immediately.
Human Doctor Final Diagnosis
Osteosarcoma