Peripheral schwannoma mimicking a bone tumour


Clinical History
A 44-year-old male patient presented with a history of several months of mechanical left shoulder pain. Physical examination showed preserved range of motion and muscle strength. The patient's past medical history was unremarkable.
Imaging Findings
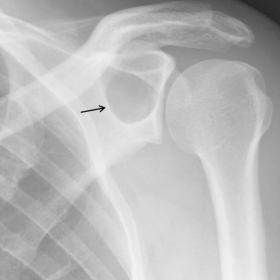
Anteroposterior radiography revealed a well-defined lytic lesion affecting the scapula. The lesion showed a narrow transition zone with a thin sclerotic rim. No cortical destruction, periosteal reaction or matrix formation was observed. (Figure 1)
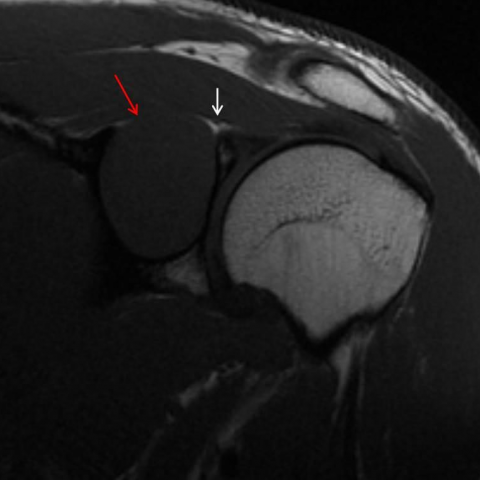
Magnetic Resonance Imaging (MRI) examination confirmed a solid, round and very well-defined soft tissue mass (3.5 x 2.8 x 2.4 cm) with epicentre in the spinoglenoid notch. There was also large remodelling of the underlying scapula that preserved a rim of very thin cortical rest.
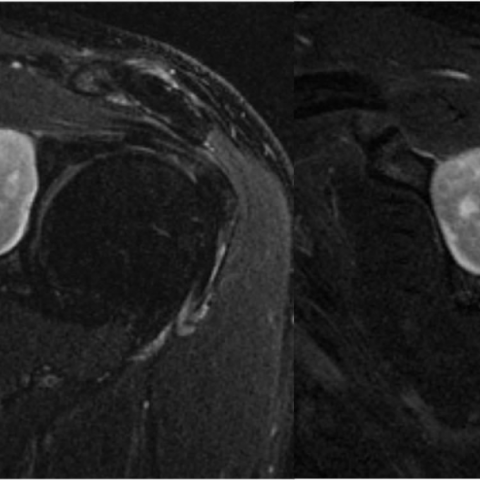
The lesion had an intermediate signal intensity on T1-weighted images (WI) (Figure 2), hyperintense on the T2-WI (Figures 3) and an homogeneous enhancement after administration of Gadolinium (Figure 4).
A close relationship between the tumor and the suprascapular nerve was observed, but contiguity of both structures was not clearly shown (Figure 2).
There was no evidence of muscle atrophy, fatty infiltration or oedema suggesting denervation.
A CT-guided biopsy yielded the diagnosis of schwannoma (Figure 5).
Discussion
Solitary benign peripheral nerve sheath tumours may be subdivided into schwannomas (neurilemmoma) and neurofibromas.
In up to 90% of the cases, both schwannomas and neurofibromas correspond to solitary lesions not associated with neurofibromatosis type 1. On the other hand, Neurofibromatosis type 1 presents almost invariably multiple neurofibromas, with visceral and deep nerve involvement and an increased risk of malignant transformation.
Schwannomas are composed primarily of Schwann’s cells and they are eccentrically located in relation to the involved nerve, presenting a true capsule composed of epineurium; they can be generally separable from the underlying nerve fibres.
In contrast, neurofibromas are centrally located, rarely encapsulated, and cannot be separated from the nerve [1, 2].
Schwannomas affect patients between 20–40 years old, and represent approximately 5% of benign soft-tissue neoplasms. They usually appear as a painless slow-growing soft-tissue mass, and symptoms may initiate when the lesion become large enough to compress the adjacent nerve [1].
MRI features of schwannomas consist of iso or low-signal-intensity lesions on T1-WI, high-signal-intensity lesions on T2-WI, and avid contrast enhancement.
The lesion generally shows fusiform shape oriented longitudinally and with tapered ends contiguous to the nerve of origin.
The lesion may show a characteristic “target sign” on T2-WI, with a central hypointense region, or the “split-fat sign” that represents a rim of fat surrounding the margins of the nerve sheath tumour, especially when it has an intermuscular location.
Imaging findings in many cases do not allow differentiation between schwannomas and neurofibromas, and the fusiform shape, the “split-fat sign”, and the “target sign” can be seen in both [3].
When the schwannomas are in close relation to a bone, it is often difficult to determine whether it is a soft tissue schwannoma involving the bone or an intraosseous schwannoma involving the surrounding soft tissues [4], but this last is less frequent. In this patient the tumour causes secondary remodelling of the bone due to the slow growing pattern.
Surgical excision is the treatment of choice for schwannomas, and the lesion is usually separable from the native nerve allowing the preservation of the rest of the nerve fibres and their function. Recurrence is rare and malignant transformation is extraordinarily unusual [1].
Take Home Points:
Soft tissue schwannoma may debut with the appearance of a benign bone solitary lesion due to its proximity to bones and its slow-growing pattern. A peripheral nerve sheath tumor may be included in the differential diagnosis of any well-defined mass in close relation to a nerve.
Differential Diagnosis List
Final Diagnosis
Schwannoma of a branch of the suprascapular nerve mimicking a bone tumor.
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Anteroposterior plain radiograph

Oblique coronal T1-WI
Axial and oblique coronal T1FAT SAT-WI with IV gadolinium

Axial CT

Oblique coronal and sagittal T2 FAT SAT-WI
Medical Imaging Analysis Report
I. Imaging Findings
Based on the comprehensive evaluation of the left shoulder X-ray and MRI images, a well-defined soft tissue mass is seen in the periscapular region (subacromial area or near the glenoid). The X-ray shows that this mass causes distinct “pressure” or “remodeling” of the adjacent scapula, with localized thinning or mild bulging of the bone, suggesting a slowly growing lesion exerting long-term pressure on the osseous structure.
MRI plain and contrast scans indicate:
1. On T1-weighted images (T1WI), the lesion appears isointense or slightly hypointense compared to muscle.
2. On T2-weighted images (T2WI), it appears hyperintense, with possible “target sign” or “split-fat sign” (i.e., a fat plane around the tumor).
3. After contrast enhancement, the mass shows marked enhancement, appearing fusiform or nearly round, with a clear boundary from surrounding soft tissues.
4. The tumor is closely related to the neural structures, but most nerve fibers are not fully involved. The mass grows eccentrically on one side of the nerve bundle.
5. The lesion grows slowly without obvious invasive changes or extensive soft tissue destruction.
II. Differential Diagnosis
-
1. Schwannoma (Neurilemmoma):
Based on the imaging features (T2 hyperintensity, potential target sign or split-fat sign, eccentric growth) and the patient’s symptoms (gradual onset, mechanical pain), a peripheral nerve schwannoma is one of the main considerations among benign peripheral nerve sheath tumors. It commonly occurs in individuals aged 20-40 years but can also appear in the 40s, often presenting as a painless or mildly painful mass. As it grows, it may lead to nerve compression symptoms. -
2. Neurofibroma:
This is also a peripheral nerve sheath tumor with imaging findings similar to schwannoma, typically showing T2 hyperintensity and the “target sign.” However, neurofibromas often grow centrally within the nerve and are more difficult to separate from the nerve fibers. In the absence of other features of neurofibromatosis type 1 (NF1), and given that this tumor has a capsule, grows eccentrically, and is relatively easy to separate from nerve bundles, schwannoma is more likely. -
3. Other Soft Tissue Tumors:
Such as lipoma, hemangioma, or other rare benign soft tissue tumors, which can present as slow-growing masses. However, their MRI characteristics differ (e.g., a lipoma appears hyperintense on both T1WI and T2WI and shows fat suppression). Moreover, this lesion’s close relationship with nerve pathways is more suggestive of a nerve-origin tumor.
III. Final Diagnosis
Considering the patient’s age (44 years), symptoms (chronic left shoulder mechanical pain), imaging findings (a soft tissue mass with a well-defined capsule, eccentric growth, easily separated from nerve fibers, T2 hyperintensity with marked enhancement), and potential intraoperative or biopsy pathology, the summary is as follows:
Most likely diagnosis: Schwannoma (Neurilemmoma, a benign peripheral nerve sheath tumor).
If a definitive diagnosis is still required, surgical resection followed by pathological examination can rule out other rare nerve-origin or soft tissue tumors.
IV. Treatment Plan and Rehabilitation
-
Surgical Treatment:
For most slowly growing nerve sheath tumors that cause symptoms or potential nerve compression, complete surgical resection is the first-line treatment. Since schwannomas usually attach eccentrically to the originating nerve bundle and have a well-defined capsule, microsurgical techniques can remove the tumor entirely while preserving nerve fibers. -
Postoperative Rehabilitation:
- Short-term Rehabilitation (1–4 weeks after surgery): Focus on reducing pain and swelling and preventing joint stiffness. Routine measures may include cold therapy (if the surgical wound is closed), using an appropriate shoulder brace or sling (according to the surgical approach and medical directives), and gentle passive range-of-motion exercises for the shoulder (flexion and abduction) within tolerable limits.
- Intermediate Rehabilitation (4–8 weeks after surgery): When pain is under control, gradually increase active range-of-motion exercises, such as “wall climbing” with fingers and light resistance exercises with elastic bands (abduction, adduction, flexion, etc.). Avoid excessive weight-bearing or overly vigorous traction; slowly improve shoulder girdle strength.
- Late-stage Rehabilitation (8 weeks and beyond): Reinforce muscle strength and functional training, including resistance exercises for the rotator cuff and scapular stabilizers. Progressively increase the resistance of the elastic band or use light dumbbells. Coordinate these exercises with modified daily activities (e.g., dressing, hair combing, carrying lightweight objects) to restore normal shoulder function.
-
Exercise Prescription (Following the FITT-VP Principle):
- Frequency: 3–5 times per week for specific shoulder exercises, which can gradually increase to daily appropriate activity based on postoperative recovery.
- Intensity: Early stages should not provoke or should only slightly provoke pain; in later stages, progressively increase resistance or repetition.
- Time: Each rehabilitation session can last 15–30 minutes, separated into segments to avoid fatigue-related injuries.
- Type: Includes range-of-motion exercises, light resistance training (elastic bands or small dumbbells), proprioception exercises, and shoulder stability training.
- Progression: As function recovers, gradually increase resistance, add more repetitions, and incorporate more complex shoulder movements. Before each progression, ensure proper tissue healing and sufficient muscle tolerance.
If the patient has osteoporosis, poor cardiopulmonary function, or other comorbidities, the training intensity and methods should be adjusted under the guidance of healthcare professionals. Any discomfort during postoperative rehabilitation should be closely monitored to ensure safety.
Disclaimer:
This report is based solely on the currently provided medical history and imaging information, aiming to offer a reference for medical analysis. The specific diagnosis and treatment plan should consider the patient’s actual condition and be finalized by a qualified clinical physician after an in-person evaluation. This report does not replace a doctor’s direct diagnosis or medical decision-making.
Human Doctor Final Diagnosis
Schwannoma of a branch of the suprascapular nerve mimicking a bone tumor.