

A 16-year-old female elite ballet dancer presented with a 6-week pain and swelling of the upper-mid lumbar spine. There was no history of previous trauma.
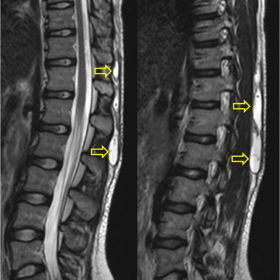
MR imaging showed a large subcutaneous well-defined fluid collection in the thoracolumbar region, superficial to the fascia (Fig. 1, 2). The lesion showed high signal intensity on fat suppressed T1W images (Fig. 3) suggesting the presence of haemorrhage. In addition, there was peripheral wall enhancement following I.V. contrast administration (Fig. 4).
A. A Morel-Lavallée lesion (MLL) is a closed degloving injury, due to an excessive shearing force or repetitive compressive trauma. The hypodermis is separated from the underlying deep fascia and a cavity filled with haematoma and lymph is formed [1, 2]. MLL is most often located at the lateral peritrochanteric region, but other sites such as the subcutaneous tissues of the abdominal wall, the buttocks, the lower lumbar spine, the scapular region, the calves and the prepatellar region of the knee may be affected [3].
B. The main symptoms of the condition are pain and swelling of the area, with clinical examination revealing a soft fluctuant area of contour deformity, with or without mobility of the skin. When damage of the cutaneous nerves occurs, hypoaesthesia near the region of trauma can also be present [4]. In chronic lesions, infection or necrosis of the underlying skin are also possible [5]. Imaging is required in order to highlight the lesion and differentiate it from other disorders.
C. Plain radiography at a MML may reveal a nonspecific soft tissue mass [5]. On ultrasound, which is the modality of choice for image-guided interventions [4], MLL appears as fluid collection with heterogeneous echogenicity, depending on the stage of evolution of the blood products. On CT, it appears as well-defined fluid collection that occasionally shows fluid levels [5]. MR imaging is the method of choice showing a low signal intensity on all pulse sequences peripheral rim. This represents the postinflammatory fibrous pseudocapsule, which may be absent in the early stages. MLL returns low on T1W and high on T2W homogeneous fluid signal intensity internally [3]. Over time, the haematoma organizes, and deoxyhaemoglobin is converted into methaemoglobin, which will show hyperintensity on T1W images [4].
D. For acute lesions conservative treatment is the first approach, including compression banding and ice. For chronic lesions, initial attempt should include percutaneous drainage with sclerotherapy. Lesions that fail this treatment or infected lesions require open drainage and secondary closure [4].
E. MR imaging is the method of choice for the diagnosis of MLL. These lesions rarely appear in the spinal region and may result from overuse.
Morel-Lavallée lesion of the lumbar region
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.




Based on the provided lumbar spine MRI (sagittal T1 and T2-weighted sequences), the following observations are noted:
Overall, the imaging findings correlate with the clinical presentation of back pain, local soft tissue swelling, and tenderness.
Considering the patient’s age of 16, her high-intensity ballet training, clinical presentation, and imaging features, the following differential diagnoses are proposed:
Taking into account the patient’s young age, high-intensity dance training, 6-week duration of symptoms, and imaging findings indicating a fluid collection with a fibrous capsule between the subcutaneous tissue and deep fascia, the most likely diagnosis is:
Morel-Lavallée Lesion (Closed Degloving Injury).
If there is still uncertainty, further assessment can be done with ultrasound or, if needed, aspiration and analysis of the lesion’s contents (blood, lymphatic fluid, or inflammatory exudate) to confirm the diagnosis.
Depending on the phase and severity, the recommended management strategies for a Morel-Lavallée lesion include:
During rehabilitation, a gradual progression (FITT-VP principle) is recommended, as illustrated below:
This report is based on the current medical history and imaging data provided and aims to offer preliminary references for healthcare professionals and patients. It is not a substitute for in-person diagnosis and treatment by a clinical physician. Please follow the advice of your healthcare provider for specific treatment decisions. If you have any concerns or changes in your condition, you should seek medical attention promptly.
Morel-Lavallée lesion of the lumbar region