Cheilitis granulomatosa: radiopathological view



Clinical History
A 19-year-old male patient presented with a year-old bilateral lip swelling, upper lip more swollen than lower lip (Fig 1). There is no history of any systemic disease, trauma, allergy, dental problem. On oral examination painless, non-tender, diffuse swelling of both lips observed.
Imaging Findings
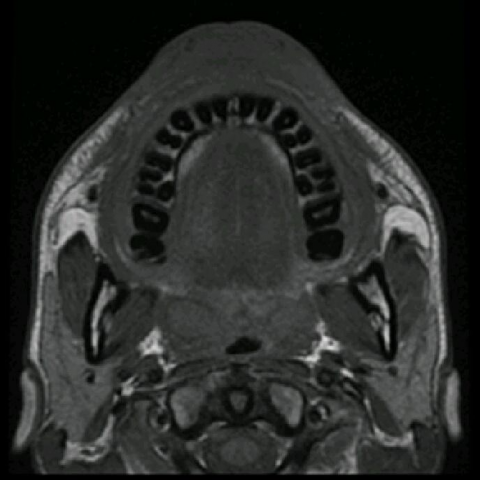
Patient referred to radiology department for imaging of face and lips. The Magnetic Resonance Imaging of the face demonstrated low-signal intensity on T1W sequence (Fig 2) and intermediate to high-signal intensity changes on T2W and STIR sequences (Fig 3 & 4). Gradient echo images indicated no bleed or vascular malformation (Fig 5). Intravenous gadolinium post-contrast study revealed homogeneous significant enhancement of thickened soft tissue of lips (Fig 6).
Accordingly, an incision biopsy of the upper lip was performed aseptically under local anaesthesia. Histopathological examination revealed ill-defined non-caseating granulomas composed of aggregates of epitheloid histiocytes with lymphocytes (Fig 7). The stroma showed dense sclerosis with hyalinisation along with focal lymphocytic infiltration. Furthermore, no evidence of necrosis or dysplasia or malignancy was seen and the section was found to be acid fast bacteria (AFB) negative. Based on clinical, imaging and histopathological evidence it is proved to be Cheilitis granulomatosa.
Discussion
Cheilitis granulomatosa (CG) is an uncommon chronic granulomatous inflammatory disease characterised by painless swelling of one or both of the lips. Dr. Miesher, a German dermatologist was the first one to describe such lesions as Cheilitis granulomatosa in 1945 [1, 2]. CG has a female predilection, affecting young adults [3]. CG is believed to be a variant of Melkersson Rosenthal Syndrome (MRS) which is a triad of recurrent orofacial soft tissue oedema, tongue plication and facial paralysis. CG is also considered as a manifestation of orofacial granulomatosis (OFG), a notion given by Wiesenfield in the year 1985 [4].
The exact cause of Cheilitis granulomatosa is unknown. The possible aetiologies discussed are hypersensitive reaction, chronic dental infections, food allergy, an association of Crohn's disease, sarcoidosis, systemic disease or hereditary angioedema [3, 5, 6]. According to Hornstein et al. CG could be due to alteration in autonomic nervous system of face leading to increased vascular permeability and oedema [7].
Within the lamina propria non-caseating granulomas with multinucleated giant cells, perivascular lymphocytic aggregates and lymphatic vessels dilatation are the usual histopathological findings associated with Cheilitis granulomatosa [5]. Long standing lesions can cause fibrosis [3].
As the differential diagnosis of lip swelling is quite lengthy, it is very important to identify the causative factor by taking proper history and thorough evaluation. Chest radiograph is done to rule out tuberculosis and sarcoidosis, look for presence of any gastrointestinal symptoms of Crohn's disease, family history of angioedema (C1 esterase inhibitor deficiency) and allergy testing for sensitive food items [5, 6, 8].
Corticosteroids have found to be effective in treating Cheilitis granulomatosa and preventing relapses [5, 9]. Radiation therapy and surgery indicated in cases which show no response to steroids and in gross disfiguring lip swelling [6, 10].
Chymoral Forte has been also proved an effective means of treatment of Cheilitis granulomatosa, thus preventing the patients from unnecessary adverse effects of steroids [11].
In our case, oral as well as intralesional steroids have been given to treat CG, and the patient responded well with no evidence of recurrence. This case report is an attempt aimed to contribute towards available radiological evidence of CG. At present due to non-specificity there are less documentary discussions available on radiological findings of CG. To summarise, as the exact aetiology of CG is not known, a detailed history, investigations along with histopathology will help to make diagnosis and early treatment of Cheilitis granulomatosa, as the features mimic other granulomatous diseases.
Differential Diagnosis List
Final Diagnosis
Cheilitis granulomatosa
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Axial T1W images of lips

Coronal and sagittal T2W images of lips.


Axial STIR image

Axial GRE image

Axial and sagittal contrast T1W images


Low and high power magnification images from lip biopsy


Patient with bilateral lip swelling

I. Imaging Findings
Based on the patient’s MRI images, there is significant swelling of the bilateral upper and lower lip soft tissues, with the upper lip more prominently affected. The swelling is diffuse, with slightly increased signal intensity and a full contour, and there is no clearly defined cystic or solid mass. Mild inflammatory signal changes are observed in the soft tissue, and there is no evidence of bony destruction or alveolar bone abnormalities. The tongue, buccal mucosa, and other oral regions show no significant lesions. Overall, the findings suggest diffuse thickening and inflammatory changes of the lip soft tissue.
II. Potential Diagnoses
Based on the above imaging findings and the patient’s clinical symptoms, the following diagnoses or differential diagnoses are considered:
- 1. Granulomatous Cheilitis (Cheilitis Granulomatosa, CG): Characterized by painless progressive swelling of both lips. MRI may show thickening of the lip soft tissue and inflammatory signals, without a well-defined mass lesion.
- 2. Melkersson-Rosenthal Syndrome (MRS): CG is the lip manifestation of this syndrome, which may also involve fissured tongue and facial nerve palsy. Clinical evaluation is required to determine if the facial nerve or the tongue is affected.
- 3. Other Granulomatous Diseases of the Orofacial Region (e.g., Sarcoidosis or Crohn’s Disease): Chronic swelling of the lips or perioral area can appear on imaging. Differentiation requires a correlation with systemic clinical manifestations and evidence of pulmonary or gastrointestinal involvement.
- 4. Idiopathic/Allergic Angioedema: If the patient has a history of allergy or specific triggers, short-term lip swelling may occur. However, in this case, the swelling has persisted for over a year, making acute episodes less likely.
III. Final Diagnosis
Taking into account the patient’s age (19 years), persistent bilateral lip swelling for one year, lack of significant pain or other systemic symptoms, and the imaging and histological findings (submucosal non-caseating granulomas, inflammatory cell infiltration, etc.), the most consistent diagnosis is “Granulomatous Cheilitis (Cheilitis Granulomatosa, CG).” Currently, there are no clinical signs of facial nerve palsy or fissured tongue, thus distinguishing it from Melkersson-Rosenthal Syndrome. If needed, tests for tuberculosis, sarcoidosis, or gastrointestinal evaluation may be conducted to rule out Crohn’s disease.
IV. Treatment Plan and Rehabilitation Program
According to the literature and clinical experience, the primary treatments for CG include:
- 1. Medication Therapy:
- Glucocorticoids: Oral or local steroid injections into the lips can effectively relieve inflammation and swelling.
- Anti-inflammatory enzymes (e.g., papain): May provide adjunctive decongestant effects for certain patients.
- Antiallergic and immunomodulatory drugs: May be considered if allergic factors or immune system abnormalities are suspected.
- 2. Surgical Management:
In cases of severe lip deformity or resistance to medical therapy, surgical intervention or radiotherapy may be considered. However, such invasive approaches require thorough evaluation beforehand.
Rehabilitation and Exercise Prescription:
- For this condition, there are no specific skeletal or joint restrictions, so exercise forms are generally not strictly limited. During periods of systemic or localized inflammation, moderate-intensity, full-body exercises are recommended, while avoiding high-intensity activities that might injure the lips.
- FITT-VP Principle Recommendations:
- Frequency: 3–5 times per week to avoid excessive fatigue.
- Intensity: Start with low to moderate intensity (e.g., brisk walking, light strength training), gradually increasing once the condition stabilizes.
- Time: Around 30–45 minutes per session, adjustable based on individual fitness level and symptom tolerance.
- Type: Aerobic exercises (such as walking on flat ground, using an elliptical) combined with low-intensity resistance training to enhance overall fitness.
- Progression: Gradually increase according to the reduction in lip inflammation and individual tolerance, avoiding sudden large increases that could lead to fatigue or injury.
- If other underlying issues or suspected comorbidities (e.g., respiratory distress, cardiac insufficiency) exist, a personalized exercise plan should be formulated with a specialist’s guidance.
- During rehabilitation, maintain proper oral hygiene and avoid repeated mechanical or chemical irritation to the lips, ensuring they remain adequately moisturized and protected.
Disclaimer: This report is based solely on the provided imaging and clinical information and is for reference only. It should not replace in-person medical consultation or professional advice. If you have any questions or need further confirmation of the diagnosis and treatment, please consult the appropriate specialist.
Human Doctor Final Diagnosis
Cheilitis granulomatosa