


A 52-year-old female patient with shoulder pain came to the emergency room after injuring her left shoulder on a bike ride. She underwent a shoulder radiograph, which was normal. Pain and limited mobility persisted after two months with conservative treatment, which led to another radiograph and MR imaging.
The first radiograph (Fig. 1) showed a normal alignment of the acromioclavicular joint and conserved intraarticular space. An opacity in the acromioclavicular space was seen, suggesting a post-traumatic haematoma. The glenohumeral joint was normal.
The second radiograph (Fig. 2) demonstrated enlargement of joint space which was not seen before and periarticular bony erosion of the distal clavicle (white arrow).
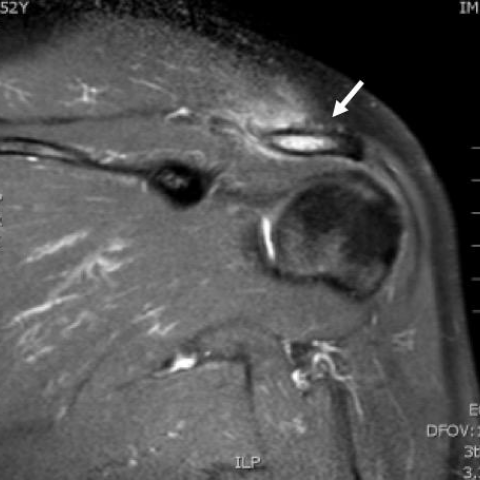
Subsequent MRI (Fig. 3) for evaluation of acromioclavicular joint confirmed periarticular erosion of the distal clavicle (orange arrow and widening of the joint capsule (Fig. 3d). An adjacent soft-tissue oedema and bone marrow oedema of the spine of scapula were also found (white arrow).
Osteolysis of the distal clavicle is a painful abnormality which may develop after an acute traumatic injury to the shoulder or may occur due to repeated microtraumata, such as the ones caused by weightlifting. [1]
In cases of distal clavicular destruction, another differential diagnosis such as rheumatoid arthritis, hyperparathyroidism, scleroderma, lytic metastasis and haematogenously spread osteomyelitis should be considered. However in cases of traumatic antecedent, this is the most probable hypothesis.
Clinically it manifests usually as pain and weakness during abduction and flexion of the arm, and it may appears weeks or years after the traumatic event. Clinical examination frequently reveals crepitus and swelling of the overlying soft tissue.
Early imaging diagnosis is difficult. In the early disease process, radiographs may be normal or only demonstrate focal soft-tissue swelling adjacent to the acromioclavicular joint. With progression of the osteolysis there is resorption and erosion of the distal portion of the clavicle which is seen as periarticular erosion and clavicular osteopenia. On the other hand acromial articular surface maintains normal morphology. [1]
MRI is the most sensible method showing loss of the normal low-signal-intensity cortical margin of the clavicle along with bone marrow oedema. Otherwise, acromion should preserve normal bone marrow signal, which is an important distinction in the differential diagnosis from septic arthritis and degenerative change. [2]
Acromioclavicular joint synovitis is usually also seen.
The pathogenesis of this entity is still unclear, however some hypotheses suggest an alteration in the vascularisation of the bone secondary to autonomic nervous system disturbance, stress fractures and avascular necrosis of the bone.
Conservative management is usually the first choice, achieving good results. When the cause is a repetitive microtrauma, as in weightlifters, cessation of the inciting activity frequently results in relief of symptoms and partial or complete osseous recovery.
In refractory cases surgical resection is performed, which is the most effective method in these cases to relieve symptoms.
Poor results were demonstrated in this condition after local corticosteroid injections or oral intake of anti-inflammatory agents. [3]
Post-traumatic osteolysis of the distal clavicle
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.





1. From the latest shoulder X-ray, it can be seen that the cortical continuity of the distal clavicle is irregular, showing localized erosion, thinning, or loss of bone (indicated by the arrow), suggesting focal bone destruction and absorption. In contrast, the acromion appears relatively normal at its margins.
2. MRI images show that the normal low-signal cortical edge of the distal clavicle is missing, with evident bone marrow edema signals (T2 hyperintensity, T1 hypointensity in the medullary cavity), accompanied by local soft tissue swelling and joint effusion. Comparing with the acromion, the acromion maintains relatively normal bone marrow signal and an intact articular surface.
3. In the acromioclavicular joint region, there is significant synovial thickening or synovitis. No clear bony destruction of the acromion is observed.
4. Based on the above imaging changes and clinical presentation, and given that symptoms have not markedly improved after two months of conservative treatment, there is a possibility that the distal clavicular lesion is progressive or remains active.
Considering the imaging features (distal clavicular osteolysis, normal acromion) along with the patient’s history of trauma and current symptoms, the following differential diagnoses should be considered:
1. Traumatic Distal Clavicular Osteolysis: Often seen after trauma or repeated micro-injuries (e.g., weightlifting). Early X-ray findings may be inconspicuous, but with disease progression, osteolysis of the distal clavicle can be noted.
2. Rheumatoid Arthritis: Can cause joint destruction and pain, typically involving multiple joints along with other systemic symptoms; imaging usually shows involvement of the acromion and other joint surfaces.
3. Metabolic Bone Diseases (e.g., Hyperparathyroidism): May present with multiple sites of bone resorption, usually not limited to the acromioclavicular joint.
4. Neoplastic or Metastatic Lesions: Lytic bone metastases could show bony destruction. However, they often occur in the context of a known primary tumor or other metastatic sites.
5. Infections of the Acromioclavicular Joint (e.g., Septic Arthritis or Osteomyelitis): Typically associated with more apparent soft tissue swelling or systemic infectious symptoms. MRI would show severe involvement of the acromion or adjacent soft tissues.
Taking into account the patient’s age, history of trauma, duration of symptoms, and imaging findings (especially the localized bony resorption in the distal clavicle with a relatively normal acromion, and MRI evidence of significant bone marrow edema without acromial involvement), the most likely diagnosis is:
Traumatic Distal Clavicular Osteolysis
Further investigations (e.g., rheumatoid factor, parathyroid hormone levels, tumor markers, inflammatory markers) may help rule out other secondary conditions. If the clinical situation is complex or a tumor lesion is suspected, a tissue biopsy could be pursued to confirm the diagnosis.
1. Conservative Treatment: Many experts advocate conservative management initially, including:
Disclaimer: This report is based solely on the provided imaging findings and clinical information and is intended for reference purposes. It does not replace an in-person clinical diagnosis or medical decision-making. If there are further questions or any changes in condition, please consult a specialist promptly.
Post-traumatic osteolysis of the distal clavicle