Distal clavicular osteolysis in a bodybuilder



Clinical History
A 33-year-old amateur body-builder presents with left shoulder pain for about 5 months, without a history of preceding acute trauma. Palpation of the acromioclavicular joint is painful. Mobilisation of the left shoulder is normal and painless.
Imaging Findings
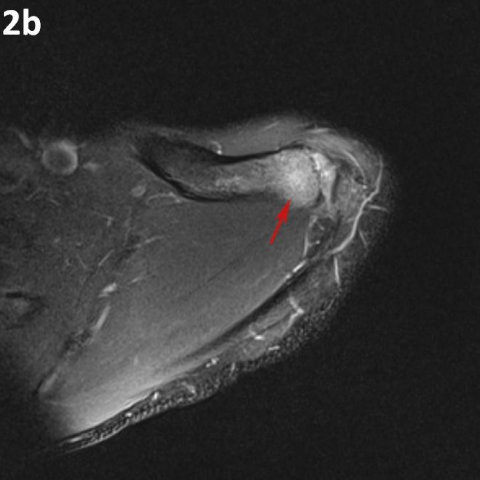
Standard radiography showed cortical irregularity of the articular side of the distal clavicle (Fig. 1a, b). The acromion appeared to be normal. The patient underwent an MR arthrography because initially rotator cuff pathology was suspected. The rotator cuff tendons and capsulolabral system were normal. There was marked bone marrow oedema in the distal clavicle while the signal of the distal acromion was almost normal (Fig. 2a, b). The subchondral cortex of the distal clavicle appeared thinned and was irregularly delineated (Fig. 2a). A mild AC-joint effusion and hypertrophy of the joint capsule was present (Fig. 2a, c). Follow-up radiographs 2 months after the initial presentation showed a normal right AC joint (Fig. 3a), whereas residual osteolysis was seen at the superolateral aspect of the left clavicle (Fig. 3b).
Discussion
Distal clavicular osteolysis (DCO) follows both chronic repetitive stress and single acromioclavicular trauma [1]. The exact aetiopathogenesis is unclear, but AC-joint trauma and subchondral microfractures seem to be involved [1, 2]. Subsequent attempts at repair are insufficient and the final result is osteolysis [1, 4]. It is unclear why changes predominate in the distal clavicle while the acromion is relatively spared [1].
DCO has been most frequently reported in weightlifters and bodybuilders [1, 2]. Overhead sports, especially when combined with supplemental weight training, are also at increased risk [4]. Professional activities requiring similar movements or exposure to chronic repetitive stress (e.g. pneumatic drill operation) can also cause DCO [5].
Clinical findings are often nonspecific and frequently overlap with those of labral or rotator cuff tears [5]. Patients experience pain in the AC-joint region, exacerbated by weight training and relieved by prolonged rest [2]. Targeted clinical examination reveals point tenderness over the AC-joint and painful cross-body adduction [2, 4].
Conventional radiographs may remain normal during the first months or years after the onset of training [1, 3]. A 15° cephalad inclination avoids superposition of the scapular spine with the AC-joint [2]. Radiographic changes include cortical thinning, irregularity and microcysts in distal clavicle and mild AC–joint widening [1, 2]. A late finding is tapering of the distal clavicle [2]. MRI is far more sensitive to detect DCO in an early stage [1]. The most common MR-finding is bone marrow oedema in the distal clavicle, sometimes also in the articular part of the acromion, but less distinct [1, 3]. Often, a hypointense line is seen in this area of clavicular bone marrow oedema, representing a subchondral fracture [1, 4]. AC-joint abnormalities are common, and include effusion, mild widening, intra-articular bone fragments and capsule hypertrophy [2, 5]. Other MR-findings are similar to those seen on radiographs, as described above.
Treatment is essentially conservative, consisting of rest and nonsteroidal anti-inflammatory drugs (NSAID's), and is usually successful [2, 4]. In severe cases, resection of the distal clavicle is indicated [1, 2]. If left untreated, the process may cause progressive resorption of lateral aspect of the clavicle, erosions and cupping of the acromion and dystrophic calcifications [3].
DCO should be considered in the differential diagnosis of shoulder pain in the appropriate population. Therefore, analysis of MR arthrographic studies of the shoulder should not be restricted to evaluation of the rotator cuff and capsulolabral system, but the AC-joint should be scrutinised as well.
Differential Diagnosis List
Final Diagnosis
Distal clavicular osteolysis
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Conventional radiograph of the left shoulder


Arthro-MRI of the left shoulder


Follow-up radiograph of both AC joints


Medical Analysis Report
I. Imaging Findings
1. X-ray images show varying degrees of irregular bone texture in the distal left clavicle (acromioclavicular joint), localized thinning of the cortical bone, and focal marginal resorption.
2. Mild widening of the joint space is observed, and there may be small cyst-like changes on the articular surface of the distal clavicle.
3. MRI reveals bone marrow edema in the distal clavicle. A low-signal band, possibly representing a subchondral fracture line, can be seen, and the joint capsule may exhibit slight thickening or fluid signals, suggesting chronic stress injury and joint degeneration.
4. Other structures within the shoulder joint, including the supraspinatus tendon and the glenoid labrum, show no significant abnormal signals. The primary lesion is focused on the junction area between the distal clavicle and the acromioclavicular joint.
II. Possible Diagnoses
Based on the above imaging findings and the history (the patient is a fitness/weightlifting enthusiast with repetitive heavy-load training), the possible diagnoses include:
- Distal Clavicular Osteolysis (DCO)
Explanation: Commonly seen in individuals who frequently lift heavy loads or repeatedly perform shoulder press movements. Prolonged chronic stress or a single joint trauma can lead to microfractures in the distal clavicle, eventually causing bone destruction. In early stages, X-rays may appear normal, but later show distal clavicular resorption and osteopenia. MRI is more sensitive in early detection of bone marrow edema and joint pathology. - Degenerative/Arthritic Changes of the Acromioclavicular (AC) Joint
Explanation: With aging or overuse, the AC joint can also degenerate, causing pain and structural abnormalities in that region. However, purely degenerative arthritis often involves articular surface sclerosis or osteophyte formation, not necessarily presenting with marked osteolysis. - Rotator Cuff or Labral Tear
Explanation: Injuries to the rotator cuff tendons or the glenoid labrum can also cause shoulder pain, but they often accompany specific activity-related issues or decreased muscle strength. In this case, joint mobility and strength assessments are relatively normal, and MRI shows no significant evidence of rotator cuff tears or labral lesions, making this diagnosis less likely.
III. Final Diagnosis
Considering the chronic shoulder strain history (weightlifting/fitness training), imaging findings of localized bone resorption in the distal clavicle, bone marrow edema, and AC joint pain, the most likely diagnosis is:
Distal Clavicular Osteolysis (DCO)
IV. Treatment Plan and Rehabilitation
1. Conservative Treatment:
- It is recommended to reduce or suspend activities that repeatedly stress or cause pain in the AC joint, especially heavy shoulder presses or bench presses.
- Oral or topical non-steroidal anti-inflammatory drugs (NSAIDs) can help alleviate inflammation and pain.
- If necessary, local physical therapy such as ice application, ultrasound, or shockwave therapy can be performed.
2. Surgical Treatment:
- If symptoms are severe or do not respond to conservative treatment, consider distal clavicle resection (AC joint arthroplasty) to relieve persistent pain and functional limitations.
- Surgical indications primarily depend on the patient’s activity demands, pain severity, and imaging findings.
3. Rehabilitation/Exercise Prescription (FITT-VP Principle):
- Frequency: Perform rehabilitation training 2-3 times per week initially, then gradually increase to 3-4 times when symptoms improve.
- Intensity: Start with low-load or bodyweight exercises, avoiding premature heavy resistance. Increase weight gradually only after significant relief of symptoms.
- Time: Each session can last 20-30 minutes, including adequate warm-up and cool-down periods.
- Type:
· In the early phase, focus on scapular stability and shoulder mobility exercises, such as scapular muscle training and band-assisted abduction/adduction exercises.
· Once pain subsides, gradually move on to functional resistance training and strength recovery exercises, such as low-load dumbbell or sandbag exercises, while avoiding overhead or excessively heavy loads.
- Progression: Increase training duration or load incrementally based on pain and recovery status. If significant pain or discomfort occurs, reduce the load or pause and seek medical evaluation.
- Volume: Recommend 8-12 repetitions per exercise for 1-2 sets to start. As symptoms subside and fitness improves, gradually increase to 2-3 sets.
4. Precautions:
- If patients experience significant limitations in daily activities or persistent pain, they should promptly revisit their doctor and undergo further evaluation.
- Those with relatively fragile bone structure or other metabolic issues need more cautious assessment before engaging in exercise.
- Patients with cardiopulmonary limitations or other chronic conditions should closely monitor heart rate and blood pressure during rehabilitation for safety.
Disclaimer
This report is a reference analysis based on current imaging and clinical information, and cannot replace in-person consultations or the face-to-face diagnosis and treatment advice of a professional physician. If you have any questions or changes in your condition, please consult an orthopedic or sports medicine specialist in a timely manner.
Human Doctor Final Diagnosis
Distal clavicular osteolysis