Pott disease (tuberculous spondylitis) (ECR 2018 Case of the Day)


Clinical History
An 81-year-old woman was treated for pyometra and at clinical examination a 6-cm ulcerating carcinoma of the left breast was discovered. She underwent mastectomy with positive sentinel biopsy. Three months later she presented with severe back pain, paraplegia and incontinence. In laboratory findings only mild CRP elevation was observed (23 mg/L).
Imaging Findings
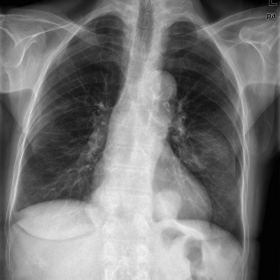
Figure 1: 6 x 3 cm mass in the left middle zone (breast tumour). Additionally paravertebral masses may be observed bilaterally.
Figure 2: Only the remaining paravertebral masses are seen.
Figure 3. Disc space narrowing and irregularity of the Th11-12 vertebral endplates.
Figure 4. Multilevel involvement and mass effect displacing spinal cord posteriorly. (A) STIR images showing hyperintense marrow (level L2 and Th 11-12) and hyperintense signal of the spinal cord at Th 11-12 level. (B) T1W images showing hypointense marrow of the affected vertebrae (mild on the level L2, pronounced on the level Th 11-12). (C) Postcontrast T1W images showing marrow, ligamentous and dural enhancement with unenhancing collections.
Figure 5. Paravertebral fluid collections (A) T2W images showing hyperintense paravertebral masses. (B) T1W images showing hypointense marrow with hypointense paravertebral masses. (C) Postcontrast T1W images showing marrow and ligamentous enhancement with unenhancing collections.
Discussion
Pott disease is also known as tuberculous spondylodiscitis and refers to vertebral body and intervertebral disc involvement with tuberculosis (TB) [1]. Spine is the most frequent location of the TB in the musculoskeletal system; commonly related symptoms are back pain and lower limb weakness/paraplegia [1]. These symptoms were as well observed in our patient. The initial working diagnosis was vertebral metastasis, however, with MRI diagnosis of spondylitis was made with suspicion of TB involvement.
Due to ability of MRI to detect marrow changes before any bony destruction, MRI plays an important role in early diagnosis even in patients with normal radiographs [2]. An important imaging feature that characterises TB infection compared to bacterial infection is sparing of the intervertebral disc in the early stage of infection [2]. Other characteristic involvement of the subligamentous spread, anterior vertebral body corner, multiple vertebral bodies, extensive paraspinal abscess formation, abscess calcification, and vertebral destruction differentiates TB from bacterial spondylodiscitis [2]. With disease progression classic discovertebral involvement may be observed and the infective process can extend into the epidural space causing cord compression.
In the presented case on the MRI characteristic findings of the Pott disease may be observed such as multilevel involvement with early involvement on the L2 vertebrae and disease progression on the level Th11-12. Furthermore, the infective process causes cord compression and paraspinal abscesses may be appreciated. The features to differentiate spondylitis from metastasis in the current case are disc involvement and pathognomonic intraosseous abscess seen on Gd-enhanced images with paravertebral extension [3].
Batson venous plexus is a network of veins with no valves that connect deep pelvic veins draining the bladder, uterus and rectum to the internal vertebral venous plexus [4]. These veins are important because they are believed to provide a route for spread of pelvic cancer metastases or infections to the spine [5]. In our case the proposed spread is a logical explanation since the patient had pyometra three months prior the clinical presentation of spinal involvement. Unfortunately sampling from pyometra procedure was not available, however, the sample taken from spondylodiscitis surgery was positive for TB and the final diagnosis of Pott disease was made. Transpedicular desis Th9-L3 with intracorporeal cage Th11-12 was made. At three years follow-up the patient shows no TB relapse or metastatic spread.
Differential Diagnosis List
Final Diagnosis
Pott disease (tuberculous spondylitis)
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Preoperative chest radiograph

Sagittal radiograph of the thoracic spine

Sagittal MR images of the spine

Axial MR images (at the Th 12 level)

Postoperative chest radiograph

Medical Imaging Analysis Report
1. Imaging Findings
Based on the provided chest and spinal X-ray and MRI images, multiple thoracolumbar vertebral bodies and intervertebral discs show involvement, along with evidence of vertebral destruction and indications of paravertebral soft tissue swelling or abscess formation. The specific findings are as follows:
- X-ray (frontal and lateral views): Some vertebral margins in the thoracic and upper lumbar regions appear irregular, and decreased vertebral height can be observed. Local suspected bony destruction and increased density in adjacent soft tissues suggest possible abscess or extension of infection.
- MRI Observations: Multiple vertebral segments (including T11–12, L2, etc.) show abnormal signals involving the intervertebral discs, exhibiting heterogeneous enhancement. Abscess-like signals are seen within some vertebral bodies and paravertebral areas, highly suggestive of infection or infiltration involving the paravertebral region and spinal canal. Relative narrowing of the spinal canal exerts some degree of pressure on the spinal cord or dural sac, corresponding to the patient’s lower limb neurological deficits (e.g., pain and paralysis).
2. Potential Diagnoses
Based on the imaging findings and the patient’s medical history, the following diagnoses or differential diagnoses are primarily considered:
- Tuberculous Spondylitis (Pott’s Disease):
- Older patient with a previous gynecological infection (pyometra), possibly spreading to the spine through Batson’s plexus.
- MRI indicates multiple vertebral bodies involved, paravertebral abscesses, and compression of the dural sac, aligning with typical features of tuberculous spondylitis.
- The intervertebral disc may be relatively less involved in the early stage of the disease, but later disc destruction—seen in this case—matches the progressive characteristics of tuberculosis.
- Pyogenic Spondylodiscitis (Bacterial):
- Can also present with vertebral destruction and paravertebral abscess, but generally the intervertebral disc is involved at an earlier stage, and clinical findings often include significantly elevated inflammatory markers (e.g., CRP, elevated white blood cell count).
- In this case, the patient’s CRP is only mildly elevated at 23 mg/L, which is atypical. Combined with the characteristic shape of the paravertebral abscess and multiple segment involvement, tuberculosis is more likely.
- Vertebral Metastases:
- The patient has a history of breast cancer, so metastatic lesions must be considered.
- Typical metastatic lesions often appear as locally osteolytic or osteoblastic changes in the vertebral body; however, severe paravertebral abscess is relatively uncommon. On MRI, diffuse enhancement may suggest metastasis, but marked intervertebral disc destruction and abscess formation are not typical for metastatic disease.
3. Final Diagnosis
Considering the patient’s history of gynecological infection, the multi-segmental involvement of vertebral bodies, and MRI findings of paravertebral abscesses and spinal canal compression consistent with tuberculous inflammation, plus positive intraoperative specimen tests confirming tuberculosis infection, the most likely final diagnosis is tuberculous spondylitis (Pott’s disease).
Surgical intervention (pedicle screw fixation, lesion debridement, and bone graft fusion, etc.) has already been performed. A three-year follow-up has shown no recurrence of tuberculosis or other evidence of metastases.
4. Treatment Plan and Rehabilitation
4.1 Treatment Overview
- Medication: Continue or complete the full course of anti-tuberculosis therapy (commonly including isoniazid, rifampin, pyrazinamide, ethambutol, etc.) for an adequate duration (usually at least 6–9 months) to consolidate control of the lesion.
- Surgical Treatment: If vertebral lesion debridement, decompression, and internal fixation have been performed, regular follow-up is required to assess the stability of the fixation and the progress of bone healing.
- Supportive Therapy: Pay attention to nutritional supplementation, use analgesics where appropriate, and consider neuroprotective agents if necessary. Manage comorbidities (such as diabetes, hypertension) as per standard guidelines.
4.2 Rehabilitation and Exercise Prescription
After the acute phase treatment and stabilization of the condition, a gradual restoration of motor function is recommended to prevent complications and improve quality of life. Given the patient’s advanced age, osteoporosis, and spinal surgery with internal fixation, special attention to safety and individualization is required.
- Early Rehabilitation (0–6 weeks post-surgery):
- Focus on protective bed rest or wearing braces, avoiding excessive forward flexion, torsion, and heavy loading of the spine.
- Gradually perform lower limb muscle-strengthening exercises such as straight leg raises (lying down or seated) and ankle pump exercises to prevent thrombosis and promote circulation.
- If ambulation is permitted, walk short distances with waist support or braces for 5–10 minutes at a time and progressively increase the number of daily walking sessions.
- Mid-Stage Rehabilitation (6–12 weeks post-surgery):
- Once internal fixation is stable and the lesion is well controlled, core muscle exercises can be introduced, such as planks (with a brace, in shorter duration and reduced intensity) and resistance or isometric training for the back muscles.
- Walking duration can be gradually extended to 15–20 minutes per session, increasing according to the patient’s tolerance.
- Avoid significant spinal rotation; if pain or other discomfort occurs, halt training and consult a rehabilitation specialist promptly.
- Late Rehabilitation (3 months post-surgery and beyond):
- Once spinal stability is ensured, aerobic exercises such as stationary cycling or swimming (after confirming spinal stability and with the doctor’s approval) may be performed 3–5 times a week, each session lasting around 20–30 minutes.
- Moderate strength and core stability training may be introduced, avoiding rapid increases in weight bearing. Under professional guidance, low-weight dumbbells or resistance bands can be used.
- Closely monitor the spinal condition and overall health status, maintain regular imaging and laboratory check-ups, and adjust the training regimen accordingly.
Throughout rehabilitation, it is advisable to follow the FITT-VP principle (Frequency, Intensity, Time, Type, and Progression) while closely monitoring disease progression. For elderly patients, special attention should be paid to cardiopulmonary function tolerance, osteoporosis, and the stability of postoperative internal fixation.
5. Disclaimer
This report is a preliminary analysis based on the current imaging and clinical reference data. It does not replace an in-person consultation or the diagnostic opinion of a professional physician. The patient and family should follow the recommendations of specialist physicians when finalizing and adjusting treatment and rehabilitation plans.
Human Doctor Final Diagnosis
Pott disease (tuberculous spondylitis)