Extraskeletal mesenchymal chondrosarcoma



Clinical History
A 66-year-old man was referred to our hospital with a slow-growing mass on his left leg. He did not report pain, weakness or weight loss. The mass was firm and the skin was intact.
Imaging Findings
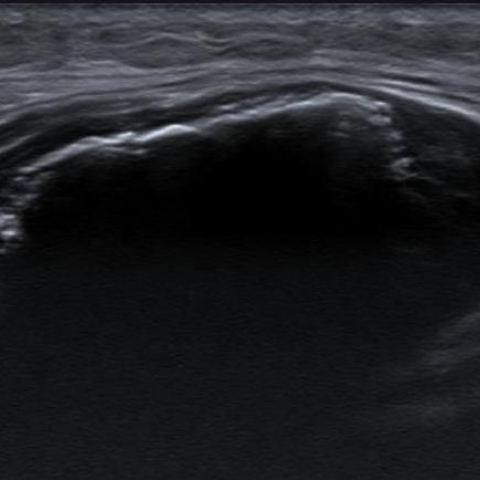
Ultrasound images show a 5 cm soft tissue mass located in the deep tissues subjacent to the superficial fascia (Fig. 1a). It appears to be densely calcified. Colour Doppler does not detect intralesional blood flow, probably due to the extensive calcification (Fig. 1b).
Conventional radiographs show a large soft-tissue mass and confirm extensive calcification (Fig. 2a, b). CT shows small, granular, streaky and amorphous calcification located in the center of the mass (Fig. 3a, b).
On MR images the central calcified area, with low intensity on both T1WI and fat-saturated DP-WI sequences, may be appreciated. The unmineralised peripheral area shows low-intermediate intensity on T1WI and high signal on fat-saturated PD-WI (Figs. 4a-d). Contrast-enhanced MRI exhibits peripheral, nodular and heterogeneous enhancement (Fig. 4d).
Discussion
Extraskeletal mesenchymal chondrosarcoma (EMC) is a rare malignancy characterised by a biphasic histologic pattern of small undifferentiated round cells and islands of well-differentiated cartilaginous matrix. It represents about 2% of all soft-tissue sarcomas [1]. The three histologic types are myxoid, mesenchymal, and low grade, which is much less frequent.
Epidemiologically, the myxoid subtype is more frequent in men around 50 years of age, whereas the mesenquimal subtype is more prevalent in young adult women [1].
Clinical presentation is nonspecific, presenting frequently as a slow-growing painless mass. In this clinical setting, radiography and ultrasound are usually the first tests requested in our institution. Depending on the findings, subsequent MRI and/or CT will be performed.
Calcification is present in about 67% of the cases [2]. Ring and arc or granular mineralisation is an important diagnostic sign, therefore CT is useful in the diagnosis, allowing analysis of the mineralisation pattern.
MRI allows to exclude fatty component and bone and vascular involvement. MRI appearance depends on the degree of calcification of the lesion.
The non-mineralised area is usually isointense on T1WI and of high to intermediate intensity on T2WI, whereas the calcified zone has low intensity on both sequences. A diffuse heterogeneous enhancement, suggesting abundant blood flow, has been reported both in the calcified and non-calcified areas [2, 3].
The differential diagnosis of EMC includes extraskeletal osteosacoma (EO), synovial sarcoma, myositis ossificans and undifferentiated pleomorphic sarcoma (malignant fibrous histiocytoma).
Dense cloud-like calcification instead of ring-and-arc mineralisation helps to distinguish EO from EMC .
Myositis ossificans usually shows rim or peripheral mineralisation after 4-6 weeks and demonstrates areas of fatty infiltration between bone trabeculae [4].
It is difficult to distinguish synovial sarcoma and undifferentiated pleomorphic sarcoma from EMC. Both of them may show erosion or invasion of adjacent bone. Synovial sarcoma usually is located around the joints [5].
Final diagnosis needs a histological confirmation, in our case an excisional biopsy was performed.
The recommended treatment of EMC is resection with wide surgical margins. The effectiveness of chemotherapy and radiotherapy remain poorly defined [6].
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Extraskeletal mesenchymal chondrosarcoma
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Ultrasound

Conventional radiographs


CT


MR images




1. Imaging Findings
Based on the provided X-ray, CT, and MRI images, there is an occupying lesion within the soft tissue of the left lower leg with a relatively clear boundary, presenting as follows:
- X-ray: A localized mass shadow can be seen in the soft tissue around the proximal and distal tibia. Within the lesion, there is prominent “ring-and-arc” and punctate, sand-like calcification. The bone structure is intact with no obvious bone destruction or reactive cortical thickening observed at present.
- CT: Axial and coronal reconstructions reveal the mass located within the muscle layer, showing heterogeneous density with high-density spots and ring-like calcifications. The lesion is relatively well-demarcated from the surrounding muscle tissue, and no significant bony erosion is observed.
- MRI: On T1-weighted images, the mass appears isointense or slightly hypointense, while on T2-weighted images it shows mixed high signal. Areas of calcification within the tumor appear as low signal on both T1 and T2 sequences. After contrast administration, the solid portions demonstrate heterogeneous enhancement, indicating a rich blood supply. No significant fat component is detected.
Overall, the imaging suggests a soft tissue occupying lesion with typical chondroid calcification. Surrounding structures are intact without obvious involvement of bone or joint.
2. Potential Diagnoses
Combining the patient’s age of 66, male, presenting with a painless progressively enlarging mass in the left lower leg, and the imaging findings showing notable chondroid calcifications, the following diagnoses should be considered:
- Myositis Ossificans: Commonly seen after trauma or repeated irritation leading to ossification within soft tissue. Early stages often show irregular calcification, which may evolve over time into a “zoning phenomenon” with a dense periphery and relatively lucent center. If the lesion is not fully matured or the morphology is atypical, it may be confused with tumor calcification, but there is usually a relevant history of trauma or chronic irritation.
- Extraskeletal Osteosarcoma: A malignant tumor arising in soft tissue that produces bone or osteoid matrix. Calcification usually appears as “cloud-like” rather than the characteristic “ring-and-arc” pattern. Given the more chondroid-type calcification observed in this case, osteosarcoma is relatively less likely.
- Synovial Sarcoma: Can appear as a soft tissue tumor arising within muscles or adjacent to joints. Sometimes involves calcification or bone erosion. It is more common in younger patients and often located near joints. In this case, the lesion shows a more typical chondroid matrix, and the patient’s age also aligns better with chondrosarcoma epidemiology, making synovial sarcoma less likely.
- Undifferentiated Pleomorphic Sarcoma (UPS, formerly Malignant Fibrous Histiocytoma): May present as a soft tissue mass with areas of necrosis or hemorrhage. Calcification is not a common feature. In this case, the “ring” and “punctate” calcification patterns inside the tumor are more suggestive of cartilaginous components.
- Chondrosarcoma (Extraskeletal Mesenchymal Chondrosarcoma and other subtypes): Clinically often manifests as a slowly enlarging, painless mass. Characteristic “ring-and-arc” or punctate calcifications are frequently observed, and imaging as well as pathology can show cartilaginous matrix. Both the imaging features and clinical symptoms in this case strongly support this diagnosis.
3. Final Diagnosis
Combining the patient’s age, clinical presentation (a painless, slowly enlarging soft tissue mass), and the imaging evidence of characteristic “ring” and “punctate” chondroid calcifications—especially if subsequent histopathological examination confirms cartilaginous matrix with a small round cell component—the most likely diagnosis is a chondrosarcoma originating outside the bone (soft tissue), such as mesenchymal chondrosarcoma.
If a definitive diagnosis is required, further histopathological examination and immunohistochemical analysis should be performed. In the absence of a conclusive pathological result, surgical or biopsy confirmation is necessary before proceeding with treatment.
4. Treatment Plan and Rehabilitation
-
Treatment Strategy:
- Surgical Resection: For a confirmed extraskeletal chondrosarcoma, wide surgical excision is the preferred treatment to ensure negative margins.
- Radiotherapy/Chemotherapy: The sensitivity of this tumor to chemotherapy and radiotherapy is still under debate. Some reports suggest that adjuvant chemotherapy or radiotherapy can be considered for larger lesions or those with unclear margins, but further evaluation of efficacy is needed.
-
Rehabilitation/Exercise Prescription:
Postoperative rehabilitation should focus on preventing scar contracture, restoring muscle strength and joint mobility, and being vigilant about potential bone and soft tissue injury. The FITT-VP principle can be applied as follows:
- Type: Emphasize joint range-of-motion exercises, strength training, and aerobic activity.
- Frequency: Early postoperative phase: 2-3 sessions per week for rehabilitation. As recovery progresses, increase to 4-5 times per week.
- Intensity: Begin with low-intensity exercises and increase gradually. Early targeted muscle strengthening can be performed under the guidance of a professional therapist using resistance bands or body-weight exercises.
- Time: Each session can start with 10-15 minutes, extending to 30 minutes or longer as tolerance improves.
- Mode: Start with gentle range-of-motion exercises and mild resistance training. Progress to functional movements (e.g., sit-to-stand, squatting), then gradually add low-impact aerobic exercises (walking, cycling).
- Progression: Increase resistance or total exercise volume as muscle strength and function recover. Monitor for pain, swelling, or functional intolerance, and adjust accordingly.
In cases where extensive tumor resection is performed, individualized rehabilitation guidance may be necessary, potentially incorporating physical therapy, electrical stimulation, or other adjunctive methods to accelerate functional recovery. Avoid high-impact exercises or those placing excessive traction on the surgical site.
5. Disclaimer
This report is prepared based on limited imaging and clinical information and is intended to provide general reference only. It cannot replace in-person consultation or formal medical advice by qualified professionals. If there are any questions or changes in the condition, please promptly consult a specialist for further examination or treatment.
Human Doctor Final Diagnosis
Extraskeletal mesenchymal chondrosarcoma