Sciatic Nerve Entrapment Neuropathy: A rare cause at a rare site



Clinical History
An 18-year-old female presented to us with complaints of a swelling in the posterior aspect of lower left thigh and pain on walking for the past ten months. On examination, no obvious lump could be seen or palpated. No deformity, color change or local rise of temperature was present.
Imaging Findings
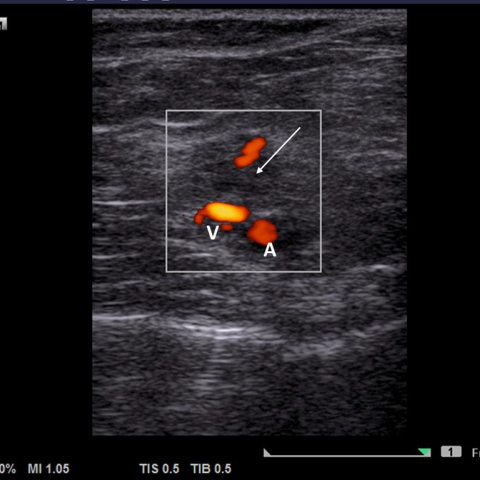
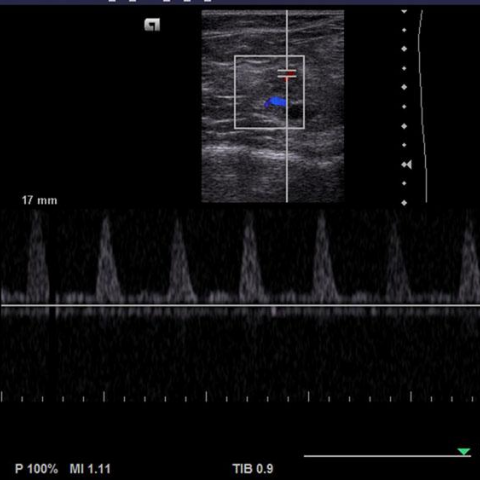
On ultrasound evaluation (Fig 1), a small hypoechoic lesion was identified in the posterior aspect of distal left thigh showing color uptake and arterial flow. Hyperechogenicity of the biceps femoris was seen suggesting fatty changes. The sciatic nerve adjacent to the lesion also appeared thickened. Hence, a provisional diagnosis of a partially thrombosed vascular malformation infiltrating distal part of sciatic nerve was made.
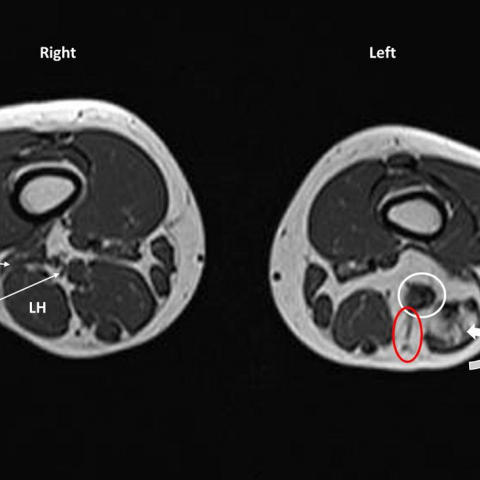
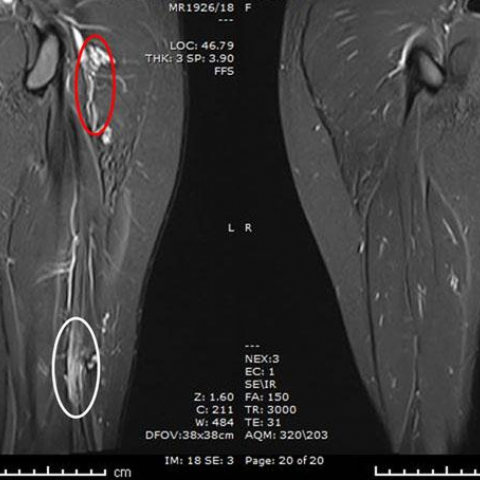
On MRI study (Fig 2), few abnormal vascular channels were seen in the posterior aspect of distal left thigh abutting the sciatic nerve. The distal part and bifurcation of the sciatic nerve showed thickening and hyperintensity with the fatty atrophy of long-head of the biceps femoris muscle. Mild thickening was also noted in proximal tibial nerve. Few abnormal vascular channels were also noted in the ipsilateral gluteal region.
Motor nerve-conduction velocity study showed reduced compound action muscle potential amplitude in biceps femoris. The sensory conduction was unremarkable.
Discussion
Background: Arterio-venous malformations (AVMs) are congenital lesions containing multiple feeding arteries and draining veins without intervening capillary bed. The main locations are head and neck (40%), extremities (40%), and trunk (20%) [1]. High-flow malformations make up approximately 10% of vascular malformations in the extremities [2][3].
Clinical Perspective: These lesions may not be evident until thrombosis, trauma, infection, local pressure effects or endocrine fluctuations occur [4][5]. They may show rapid growth over a short period of time [6]. They can present as a warm mass with an audible bruit due to high blood flow within. Bone overgrowth or arterial steal phenomenon may occur when they invade the joints [1].
Imaging perspective:
Doppler ultrasonography is the primary imaging modality required to evaluate the nature, extent and complexity of the malformation. Radiographs have a limited role and may show phleboliths indicating hemangioma or venous malformation.
High-flow AVMs can present as mixed echogenicity lesions with feeding vessels. Color Doppler and spectral analysis can be used to characterize the flow pattern. Arterialization of veins may produce pulsatile venous flow, confirming Arteriovenous shunting [7]. However, ultrasonographic assessment of deep lesions, especially those adjacent to the bone, can be challenging [8].
Computed tomography is fast and can identify complications such as acute hemorrhage, calcification and thrombosis. However, because of ionizing radiation and the minimal flow velocity information provided, its role is limited to the emergency presentations, equivocal MRI findings or as an adjunct to interventional or surgical planning [9].
MRI with Angiography shows signal voids due to high-flow feeding arteries and draining veins which appear as high-signal-intensity foci on GRE images. Early venous filling is typically seen in AVMs and contrast rise within 5–10 s is expected [3]. MRI has the added advantage of identifying multiple lesions and their relation with surrounding structures such as nerve entrapment in this case.
Outcome: Percutaneous sclerotherapy or trans-arterial embolisation are the management options for AVMs [9]. However, since these may lead to necrosis/ fibrosis of the adjacent soft tissue and nerve, surgical release of the entrapped nerve is recommended in this case to avoid long-term neuro-muscular complications.
Take home message: Our case highlights the importance of complete anatomical survey of the area under evaluation in cases of suspected AVMs. This may give an important lead for reaching a diagnosis and deciding the management options.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Partially thrombosed AV-Malformation causing sciatic entrapment neuropathy
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
High resolution USG of posterior aspect of distal thigh



MRI of Thigh



Medical Imaging Analysis Report
I. Imaging Findings
1. Ultrasound Doppler Examination:
• No obvious low- or high-echo solid mass was seen in the superficial posterior thigh; only multiple vascular structures were observed in certain cross-sections.
• Color Doppler showed high-velocity arterial blood flow signals and early venous flow changes, suggesting abnormal shunting between arteries and veins; some vessels had pulsatile flow velocity waveforms consistent with the characteristics of “arterialized” veins.
• Imaging of nerve bundles adjacent to and within deeper structures caused some interference with ultrasound assessment, but the sciatic nerve appeared to be in close proximity to the abnormal vessels.
2. MRI and MRA (Magnetic Resonance Angiography):
• Multiple “signal void” vascular structures were visible on T1-, T2-weighted, and GRE sequences, indicating fast-flow arteriovenous channels.
• Contrast-enhanced images showed venous signal enhancement within 5–10 seconds, consistent with a high-flow pulmonary arteriovenous malformation (AVM).
• The sciatic nerve was compressed or displaced near the lesion, suggesting that local nerves might be encircled or compressed by the abnormal vascular bundle.
• No significant muscle or bone destruction was noted, but considerable involvement of the local soft tissue spaces was observed.
II. Possible Diagnoses
- Arteriovenous Malformation (AVM)
- Venous Malformation or Hemangioma (e.g., Cavernous Hemangioma)
- Other Soft Tissue Tumors or Vascular Lesions
• Basis: Presence of multiple high-velocity arterial flows and early venous opacification; Doppler and MRI reveal a high-flow vascular cluster, typical of high-flow vascular malformations.
• Pathogenesis: Congenital or acquired local vascular abnormalities forming arteriovenous shunts, often leading to nerve or soft tissue compression.
• Basis: If purely venous in nature, Doppler would indicate low-flow venous patterns; however, in this case, there is a significant arterial component, making this less likely.
• Pathogenesis: Often due to congenital vascular developmental abnormalities, typically characterized by slower flow, and can present with thrombosis or calcification.
• Basis: Malignant soft tissue tumors (e.g., sarcomas) on MRI often present with heterogeneous enhancement and tissue changes, but in this case, the main imaging feature is the vascular cluster and abnormal flow velocity.
• Pathogenesis: Such tumors usually show local soft tissue destruction or a mass effect, but these findings are not typical in this case.
III. Final Diagnosis
Considering the patient is a young female with persistent swelling and pain in the posterior thigh, and both ultrasound and MRI revealing a high-flow vascular anomaly with early venous filling, plus the likelihood of local nerve structure (sciatic nerve) involvement, the most probable diagnosis is:
High-flow Arteriovenous Malformation (AVM) with Sciatic Nerve Compression
If further confirmation or assessment of lesion extent is needed, angiography (DSA) can be performed to clarify the distribution of feeding arteries and draining veins.
IV. Treatment Options and Rehabilitation Plan
1. Treatment Strategy:
• Endovascular Intervention: Includes percutaneous sclerotherapy or arterial embolization to reduce blood flow in the malformed vessels. This method can effectively control bleeding and reduce lesion size but must be performed with caution in deep structures to avoid complications involving nerves and muscles.
• Surgical Intervention: For patients with significant symptoms or severe nerve compression, surgical resection or ligation of the abnormal vessels may be considered, along with decompression of nerves that are encircled or compressed, to alleviate pain and prevent potential nerve dysfunction.
• Comprehensive Treatment: A combination of endovascular procedures and surgery, sometimes supplemented with intraoperative or postoperative sclerotherapy, may improve the cure rate and reduce the chance of recurrence.
2. Rehabilitation/Exercise Prescription:
Based on the patient’s current symptoms (pain when walking, possible nerve compression) and the nature of the vascular malformation, exercise plans should be initiated once the lesion is relatively stabilized or decompressed.
• Acute Phase or Initial Treatment Phase
▪ Frequency: Gentle activity 1–2 times per week is recommended to avoid excessive traction on the affected nerve.
▪ Intensity: Maintain low-load activities (e.g., small-range passive or active joint movements), avoiding vigorous exercise.
▪ Duration: 10–15 minutes per session, monitoring subjective pain and local conditions at all times.
▪ Type of Exercise: Focus on mild flexion-extension exercises for the lower limb, such as leg raises and knee joint movements in a sitting or supine position, along with gentle massage of the leg (avoid direct pressure on the lesion area).
▪ If the patient experiences significant neuralgia or localized swelling, reduce activities and consult a specialist promptly.
• Chronic Recovery Phase or Postoperative Rehabilitation
▪ Frequency: Gradually increase to 3–4 times per week, adjusting based on tolerance and medical evaluation.
▪ Intensity: Progress from low to moderate intensity; light resistance exercises using elastic bands can be added, taking care to avoid excessive load on the lesion area.
▪ Duration: Extend to 20–30 minutes per session, adjusting according to subjective comfort.
▪ Type of Exercise: Gradually introduce low-impact aerobic exercises (e.g., swimming, cycling) and begin core stability training to reduce reliance on the lower limbs alone.
▪ Progression: In line with pain relief and guidance from a physical therapist, progressively incorporate strength training and flexibility exercises, while still avoiding excessive stretching or impact to the affected area.
• Safety Precautions:
▪ Avoid excessive fatigue and impact during exercise to prevent vascular rupture or increased nerve compression.
▪ If pain or swelling worsens, discontinue training and seek medical advice promptly.
▪ Tailor the plan to individual differences. If the patient has other systemic illnesses or limited physical capacity, consult specialists to develop a customized rehabilitation program.
Disclaimer:
This report provides a reference analysis based on existing imaging and clinical information and does not replace an in-person consultation or professional medical advice. In case of further questions or changes in condition, please seek prompt medical evaluation or consult the appropriate specialist.
Human Doctor Final Diagnosis
Partially thrombosed AV-Malformation causing sciatic entrapment neuropathy