Popliteal Amyloidoma



Clinical History
A 63-year-old woman with a history of a resected popliteal mass years ago, is referenced to our institution for a 6 cm slow-growing mass, located in the left popliteal fossa, associated with pain and local functional disturbance.
Firstly, an ultrasound was requested, followed by an MRI and a PET-CT scan.
Imaging Findings
Ultrasound revealed a solid hypoechogenic lesion in the left popliteal fossa, with lobulated well-defined contours and no evident vascularization.
Magnetic Resonance Imaging (MRI) better evaluated the extent of the tumour, demonstrating 3 individualized lesions along the popliteal fossa, the bigger located in the supra-genicular plane. All of them revealed lobulated well-defined contours, separated from the adjacent structures without infiltration/invasion of them, only exerting mass effect. All lesions demonstrated iso-intensity to muscle on T1-weighted images, heterogeneous markedly hypo-intensity on T2-weighted images, no restriction on diffusion-weighted images, some oedema represented by discrete hyper-intensity on T2-SPAIR images, and a slight homogeneous enhancement after gadolinium administration on T1-3D Fat Suppression dynamic acquisition.
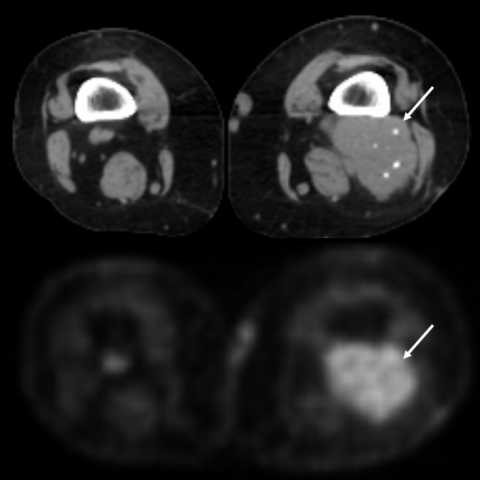
PET-CT demonstrated some punctiform dispersed calcifications within the lesions, a density similar to muscle, and a Standardized Uptake Value (SUV) of 4,49. No other lesions were documented.
Discussion
Amyloidosis includes a group of diseases where there is extracellular deposition of amyloid, a unique proteinaceous insoluble material, resistant to proteolysis.[1,2] The deposition may be systemic, organ-limited or localized, and the disease can be hereditary or acquired.[3] Classification is based on the type of protein fibril (25 types already identified), the most common being amyloid light chain (AL type) and serum amyloid A (AA type).
The rarest presentation is in the form of a tumoural mass of amyloid deposition without systemic amyloidosis, called amyloidoma, which can be present in many anatomic sites.[2] In the soft-tissue subgroup, amyloidomas of the extremities are considered exceptional. The largest series of soft-tissue amyloidomas included 14 cases, none of which in the limbs.[4]
Clinically, they present as a slow-growing soft-tissue tumour, with local mass-effect in the adjacent structures, which can be associated with pain, functional disturbance and even vascular compromise.[5] These findings, however, are non-specific.
In the popliteal fossa, the origin of an amyloidoma is thought to be the result of chronic synovial inflammation, with consequent deposition of AA amyloid type in a synovial cyst similar to a Baker’s cyst.[5]
Attending to its rarity, imaging characteristics are not well known, with only a hand-full of case reports describing its signal on MRI.[3,5,6] On CT, amyloidomas frequently reveal foci of punctiform calcifications, which can increase the suspicion of an amyloidoma.[7] On T1W the signal is iso-intense to muscle, on T2W the signal is described as hypo-intense, with mild inhomogeneity, and on post-contrast T1W the tumour mildly enhances homogeneously.[3,5,6] However, at least one case report of a thigh amyloidoma revealed a heterogeneous lesion with areas of hyper-intensity, both on T1W and T2W,[1] which makes the signal characteristics not specific for diagnostic purposes. Regarding its borders/contours, a range of presentations from well-defined, regular or lobulated, to infiltrative and irregular have been described.[1,3] Regarding PET-CT, some case reports have described SUVs under 5,[8] while others mentioned SUVs over 5.[9,10]
Treatment of choice is based on surgical excision, with no adjuvant therapy, since is a benign non-metastatic tumour. This principle is also valid for local recurrences.[1]
Peripheral soft-tissue amyloidoma is a rare localized presentation of amyloidosis, usually with local pain and functional disability, with no typical imaging findings, being diagnosed only after a biopsy, and treated with surgical excision.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Multifocal Recurrent Popliteal Soft-tissue AA type Amyloidoma.
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Ultrasound in B-mode and Colour Doppler evaluation


Sagittal T1W-SE and T2W-TSE images


Coronal T1W-SE images of the popliteal fossa


Axial T2-SPAIR image of the supra-genicular lesion

Axial DWI images through the biggest, supra-genicular lesion


Whole body 18-FDG PET-CT


Sagittal T1-3D Fat Suppression image after gadolinium administration

Medical Imaging Analysis Report
I. Imaging Findings
Based on multi-modal imaging data, including ultrasound, MRI, and PET-CT, a soft tissue mass approximately 6 cm in diameter is observed in the left popliteal fossa. Ultrasound shows a lesion with relatively hypoechoic characteristics, well-defined margins, and heterogeneous internal echoes. On MRI, T1WI indicates isointensity or slightly low signal compared to muscle, while T2WI mostly demonstrates relatively low signal, with mild mixed signal in certain regions. After contrast enhancement, the lesion exhibits mild to moderate homogeneous enhancement, with scattered punctate calcifications or high-density foci. The lesion is closely related to nearby muscles, the joint capsule, and ligaments, causing localized compression of adjacent structures and functional impairment. PET-CT reveals moderately increased metabolic activity, with SUV values ranging from about 4 to 5.
II. Potential Diagnoses
- Soft Tissue Amyloidoma:
This condition is caused by localized amyloid protein deposition, often presenting as a slowly growing soft tissue mass that may contain calcifications. MRI signals can be complex, with low signal on T2WI considered typical for some cases, although heterogeneous signals can also occur. PET-CT may show moderate uptake. - Baker’s Cyst (Popliteal Cyst):
Typically presenting as a synovial cyst behind the joint cavity, T2WI usually shows high signal, and the cyst wall may display limited thickening or enhancement. However, it generally appears as a fluid-density or fluid-signal lesion, often accompanied by concurrent joint pathology. - Malignant Soft Tissue Tumor (e.g., Synovial Sarcoma or Liposarcoma):
Malignant tumors often exhibit irregular, infiltrative borders, significant enhancement or necrotic areas, and greater metabolic uptake (higher SUV values). However, in this case, the SUV is not particularly high, and the slow course along with the imaging findings do not strongly suggest malignancy.
III. Final Diagnosis
Considering the 63-year-old patient, the long disease course with slow growth, local pain and functional impairment, the MRI findings of relatively low T2WI signal with mild enhancement, and a moderately elevated PET-CT SUV value of around 4–5, pathology indicates localized amyloid deposition. Combining all clinical and imaging evidence, the most likely diagnosis is localized soft tissue amyloidoma (soft tissue amyloidoma).
If the diagnosis remains uncertain, further histopathological examination and immunohistochemistry can be conducted for confirmation.
IV. Treatment Plan and Rehabilitation
1. Treatment Strategy:
- Surgical Treatment: The current preferred approach for soft tissue amyloidoma is complete surgical resection, especially for larger masses causing significant symptoms.
- Pathological Follow-Up: Postoperative histological and immunohistochemical assessments are important to identify the type of amyloid and to rule out systemic amyloidosis.
- Other Adjuvant Therapies: If there is no systemic amyloidosis, no specific medication is necessary. Some patients may opt for symptomatic treatment, such as analgesics or medications that reduce local edema, as needed.
2. Rehabilitation and Exercise Prescription:
After surgical management, rehabilitation training can help reduce popliteal and surrounding joint mobility limitations, accelerating functional recovery. Under the guidance of specialists or physical therapists, a gradual rehabilitation plan is recommended as follows:
- Early Stage (2–4 weeks post-surgery):
- Gentle knee range-of-motion exercises: For example, practicing knee flexion and extension in bed, guided by pain tolerance, starting with small ranges to avoid excessive stretching.
- Low-intensity muscle strengthening: Isotonic or isometric exercises for nearby muscles such as the quadriceps and gastrocnemius to gradually enhance muscle strength.
- Frequency and duration: 1–2 sessions per day, each lasting 10–15 minutes, combined with relaxing practices like ankle pump exercises.
- Mid Stage (4–8 weeks post-surgery):
- Increasing range-of-motion exercises: For example, seated or standing knee flexion and extension.
- Enhancing strength and stability: Light weights or resistance bands can be used for quadriceps and hamstring exercises.
- Frequency and duration: 3–4 sessions weekly, each lasting 20–30 minutes, alternating between knee and ankle functional training.
- Late Stage (beyond 8 weeks post-surgery):
- Progressive weight-bearing exercises: Squats, step-ups, and similar exercises to improve knee stability.
- Walking or light jogging: If recovery allows, start with low-impact surfaces or a treadmill, gradually increasing intensity.
- Frequency and duration: 3–5 sessions per week, each lasting 30–45 minutes, with volume progressively increased.
Throughout the rehabilitation process, attention should be paid to wound healing, pain, and local swelling. If symptoms worsen significantly, consult a physician promptly to adjust the training plan.
Disclaimer:
This report is a reference-based analysis derived from the available clinical and imaging information. It does not replace in-person consultation or professional medical advice. Specific treatment and rehabilitation plans should be developed and guided by a qualified physician or physical therapist according to the patient’s actual condition.
Human Doctor Final Diagnosis
Multifocal Recurrent Popliteal Soft-tissue AA type Amyloidoma.