Acute Schmorl Node in Lumbar Spine: An Unusual Cause of Back Pain



Clinical History
A 48-year-old woman presented with severe low backache for 7 days before. Pain was nocturnal and increased with movements. The patient had no previous history of trauma and no neurological abnormalities were noted. She had a medical history of breast cancer.
Imaging Findings
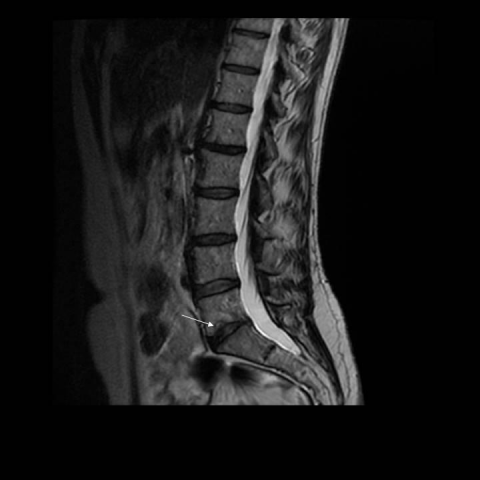
MR images demonstrated a defect with concentric rim of oedema (hypointense in T1, hyperintense in T2 and STIR) in the inferior endplate of L5 vertebra in relation to herniation of disc material (figures 1a, 1b, 1c) After contrast, there was enhancement of the lesion (figure 2). In addition, there was loss of height and signal intensity of the L5-S1 disc. No fractures, soft tissue masses or either significant findings were observed.
The imaging findings were consistent with small Schmörl hernia with acute inflammatory changes.
Discussion
Schmörl nodes, classically known as intravertebral disc herniations, were first described by Schmörl. It represents a herniation or an extrusion of the intervertebral disc nuclear material through the vertebral body endplate, with displacement of this material into the adjacent vertebral body [1]. Generally, the Schmörl nodes are considered to be a common an assymptomatic incidental finding on imaging, especially around the thoracolumbar junction [1, 2, 3]. However, Schmörl nodes , or acute cartilaginous node, can rarely manifest with acute symptoms, most common in the mid to lower lumbar spine [2,3] .
Schmörl nodes in an active phase are characterized by an area of oedema-type T1-hypointense and T2- hyperintense signal intensity in the adjacent vertebral body surrounding the node; this area may have a concentric morphologic structure.
After the administration of gadolinium-, the disk and the peripherally oedema enhance homogeneously for 6 months or more [2].
The differential diagnosis should include infective spondylitis or neoplastic lesion, but acute Schmörl node can be diagnosed by demonstrating herniated disc content, osseous defect involving single end plate, marrow focal edema around the herniated disk (concentric halo) and lack of diffuse disk signal change. The clinical features of infection, a paraspinal or epidural soft-tissue mass and paraspinal inflammatory changes [2] can help the diagnosis of infective spondylitis.
Management is usually conservative; bed rest, analgesics and bracing being the mainstay of treatment [2, 3].
Take Home Message:
Schmörl nodes or intervertebral disc herniations are commonly seen as an incidental finding on imaging, and they are often assymptomatic. However, acute Schmörl node is a rare entity, that should not be confused with tumour or infection [1].
‘Written informed patient consent for publication has been obtained.’
Differential Diagnosis List
Final Diagnosis
Acute Schmörl Node
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Sagittal MRI of lumbar spine


Sagital post-contrast gadolinium MRI

Medical Analysis Report
I. Imaging Findings
This MRI study (including T1-weighted, T2-weighted, and contrast-enhanced scans) primarily demonstrates the protrusion of disc material from the vertebral endplate into the vertebral body in the lower lumbar spine (indicated by the arrow in the images), with mild osseous defects at the corresponding vertebral endplate. The surrounding vertebral marrow shows low signal on T1WI and ring-like or band-like high signal on T2WI, suggesting edema or inflammatory response. After contrast enhancement, mild to moderate enhancement is observed in the protruded disc region and the surrounding edematous area, with no obvious epidural or paravertebral soft tissue mass.
The patient has a history of breast cancer. However, no obvious widespread vertebral destruction or extensive soft tissue lesion is observed in this imaging study, which does not fully align with vertebral metastasis or infectious lesions.
II. Potential Diagnoses
- Acute Schmorl’s Node (intra-vertebral herniation of the nucleus pulposus)
- Typical imaging features include protrusion of the nucleus pulposus through the vertebral endplate, with a ring-like or band-like edema zone showing low signal on T1WI and high signal on T2WI.
- Local pain can occur, and mild vertebral edema with enhancement may be observed around the lesion.
- Infectious Spondylitis (e.g., Pyogenic Spondylitis, Discitis)
- Usually accompanied by significant paravertebral soft tissue edema or abscess, with extensive destruction of the vertebral body and intervertebral disc.
- Clinically, fever and elevated white blood cell count and inflammatory markers (e.g., CRP, ESR) are often noted.
- Vertebral Metastasis
- Given the patient’s history of breast cancer, the possibility of bone metastasis should be considered.
- Typical findings include low- to intermediate-signal or mixed-signal destruction of the vertebral body, potentially accompanied by vertebral structural damage and soft tissue masses.
III. Final Diagnosis
Considering the patient’s symptoms (acute severe back pain without a significant history of trauma), imaging features (localized involvement of a single vertebral endplate, T1 low, T2 high signal ring-like edema zone, and characteristic enhancement), and the absence of extensive vertebral destruction or soft tissue mass despite a history of breast cancer, these findings are more consistent with an “acute Schmorl’s node (intra-vertebral disc herniation).” If there remains a high clinical suspicion of infection or tumor, further evaluation with serum inflammatory markers (e.g., CRP, ESR) and imaging such as bone scan or PET-CT is recommended to rule out infection or metastasis.
IV. Treatment Plan and Rehabilitation
1. Treatment Strategy
- Conservative Treatment: For acute Schmorl’s node, bed rest is usually recommended along with oral or topical analgesics (e.g., NSAIDs) to relieve pain. The use of a brace (lumbar support) can help reduce vertebral load.
- Medication: In the absence of evidence of infection or metastasis, standard pain relievers and anti-inflammatory drugs are typically sufficient. When necessary, muscle relaxants or neurotrophic drugs may be used to alleviate symptoms.
- Surgical Indication: Surgery is considered only if severe neurological symptoms develop (not currently observed) or if conservative treatment is ineffective, with the goal of decompressing and repairing the affected vertebral tissue.
2. Rehabilitation/Exercise Prescription (FITT-VP Principle)
Since Schmorl’s node can present with local pain and inflammatory reactions, early management focuses on pain control and basic functional recovery, gradually transitioning to core muscle strengthening to reduce the risk of re-injury. The following progressive recommendations may be considered:
- Frequency: 3–5 times per week, adjusted flexibly based on pain levels and physical capacity.
- Intensity: Engage in low-intensity aerobic and stretching exercises within a tolerable pain threshold. Begin at approximately 30%–40% of maximal effort, gradually increasing to 50%–60%.
- Time: Start each session at 15–30 minutes. As recovery and endurance improve, extend duration to 30–45 minutes.
- Type:
- Early Stage: Simple supine core stabilization exercises (e.g., pelvic lifts or small-range bridge exercises), gentle back muscle training.
- Later Stage: Introduce mild lumbar stretches or “cat stretch,” swimming, cycling, or other activities that do not excessively load the lumbar spine.
- Volume/Progression:
- Gradually increase the number of repetitions and duration. For instance, start with 10 reps per set, 1–2 sets per day, and progress to 15–20 reps, 2–3 sets per day.
- After symptoms improve, incorporate light resistance exercises or core-strengthening workouts (e.g., plank), but avoid high-impact activities or exercises that heavily stress the lumbar spine.
It is also important to assess bone quality and cardiopulmonary status. In cases of osteoporosis or other comorbidities, exercises should be performed under the guidance of a qualified physician or rehabilitation therapist to prevent secondary injury.
Disclaimer: This report is a reference-based analysis derived from the available examination data and clinical information. It should not replace in-person medical consultation or the advice of a qualified physician. If you have any doubts or your symptoms worsen, please seek prompt medical attention.
Human Doctor Final Diagnosis
Acute Schmörl Node