Pseudoaneurysm of the posterior tibial artery associated with an Achilles tendon injury: An unexpected finding



Clinical History
A 52-year-old gentleman, with hypertension and atrial fibrillation (anti-coagulated with apixaban), presented with left-calf pain following a fall into a badger hole. Clinical examination showed gross swelling of the left calf, loss of ankle plantar flexion, and positive Simmonds# test. An ultrasound of the left calf was arranged.
Imaging Findings
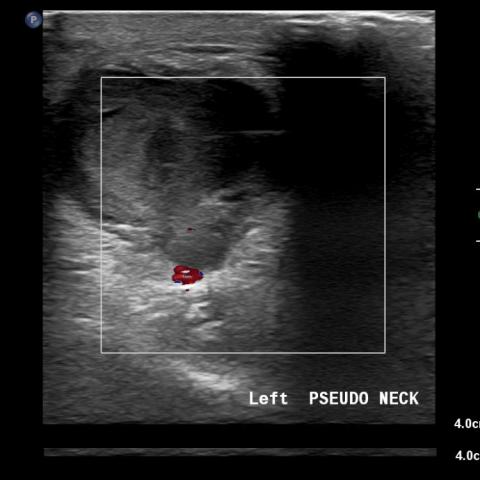
Initial duplex ultrasound of the left calf showed a partial thickness tear of the left Achilles tendon. Deep to the tendon at its anterior mid-portion, a vascular lesion was seen visible with a characteristic ying-yang sign in keeping with pseudoaneurysm (Fig. 1). A subsequent CT angiogram revealed the pseudoaneurysm arising from a small perforating branch of the posterior tibial artery, measured 28 x 23 x 48 mm with a small arterial enhancing lumen measuring 17 x 14 x 13 mm (Fig. 2). An MRI confirmed the presence of a partial-thickness Achilles tendon rupture, with 70% fibre disruption (Fig. 3).
Following consultation in interventional radiology, the patient underwent ultrasound-guided thrombin injection (0.2ml) into the pseudoaneurysm resulting in complete thrombosis (Fig. 4). The patient was managed conservatively for the Achilles tendon injury.
Discussion
Pseudoaneurysm of the crural arteries is a rare condition, predominately caused by iatrogenic intervention, trauma, or collagen vascular disorders [1-3]. A review of the literature demonstrates this is the first case to describe a pseudoaneurysm associated with an Achilles tendon tear following blunt trauma. In this case, the patient denied any previous percutaneous instrumentation or endovascular treatment. There were no identifiable risk factors for a collagen vascular disorder. The patient did report past repetitive football-related injuries.
Duplex ultrasonography is the mainstay imaging modality for diagnosis and evaluation of an extremity pseudoaneurysm. The pseudoaneurysm demonstrates a characteristic ‘to and from’ Doppler waveform on ultrasound, described as the ying-yang sign [4]. CT angiogram may be used for further evaluation when ultrasound is inconclusive or endovascular treatment is planned. In this case, extensive soft tissue oedema limited sonographic evaluation of the origin of the pseudoaneurysm and a CT was performed.
Contained by the adventitia and perivascular soft tissue, small pseudoaneurysms may undergo spontaneous thrombosis and can be managed conservatively. However larger lesions are often symptomatic and in the setting of continuous anticoagulation, as in this case, usually require treatment to prevent enlargement, rupture and subsequent potential leg ischaemia. Treatment options range from ultrasound-guided compression, thrombin injection, endovascular coiling or stenting, and surgical ligation when the limb is threatened [5]. Following discussion with our vascular surgery colleagues and consultation with the patient, thrombin injection under ultrasound guidance was performed with an excellent outcome as confirmed on repeat ultrasound with near complete absence of flow at the aneurysm neck. There were no adverse clinical sequelae, and the patient made a good recovery.
In conclusion, pseudoaneurysm of the lower crural arteries is a rare entity following blunt trauma. Initial investigation with ultrasound is recommended in all patients with symptomatic calf swelling which may reveal the presence of a characteristic vascular lesion or guide further evaluation with cross-sectional imaging. Treatment should be evaluated on a case-by-case basis, following multi-disciplinary discussion with interventional radiology and vascular surgery, as well as appropriate consultation with the patient.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Pseudoaneurysm of left posterior tibial artery associated with Achilles tendon tear
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures



Medical Imaging Comprehensive Analysis Report
I. Imaging Findings
1. Ultrasound (Color Doppler): A cystic abnormal low-echo lesion is observed in the posterior region of the left lower leg adjacent to the Achilles tendon. The color Doppler flow inside shows a “to-and-fro” or “swirling” pattern (commonly referred to as the “yin-yang sign”), indicating communication with the arterial system. A narrow “neck” connecting to an arterial branch is visible, consistent with a pseudoaneurysm. Significant surrounding soft tissue swelling and local exudation are noted.
2. CT (Angiography): A cystic abnormal enhancement connected with an arterial branch is seen in the deep soft tissue of the left lower leg, surrounded by tissue swelling and exudation. The boundary of the pseudoaneurysm is relatively clear, but due to significant local edema, the exact origin of the vessel is difficult to determine.
3. MRI: Sagittal and axial sequences indicate discontinuity and abnormal signal in the left Achilles tendon, consistent with Achilles tendon tear. Marked soft tissue edema is observed in the local area, and possible hematoma or vascular lesion signals are noted nearby. Taken together with the above findings, these are suggestive of a pseudoaneurysm.
In summary, the most prominent imaging feature is the formation of a pseudoaneurysm in the posterior aspect of the left lower leg near the Achilles tendon, accompanied by signs of Achilles tendon rupture/tear. Significant local soft tissue edema is consistent with a post-traumatic syndrome.
II. Potential Diagnoses
- Pseudoaneurysm: Based on the “to-and-fro” flow pattern observed on color Doppler and the history of trauma, there is a high suspicion of partial arterial wall rupture contained by surrounding soft tissue or remnant external membrane, leading to the formation of a pseudoaneurysm.
- Local Hematoma with Vascular Leakage: Common after trauma; however, if the ultrasound and CT angiography do not show communication between an arterial branch and the hematoma, it is more likely to be a simple hematoma. The current imaging characteristics of blood flow strongly support a pseudoaneurysm.
- Achilles Tendon Tear with Peritendinous Hematoma: Although Achilles tendon injury is confirmed, a simple tendon tear does not usually present with the “to-and-fro” flow pattern. If there is arterial communication, pseudoaneurysm remains the primary consideration.
Considering the patient’s history of trauma (fall) and ongoing anticoagulation therapy, along with the imaging findings, the first diagnosis stands out as the most likely.
III. Final Diagnosis
Taking into account the history of injury, the findings on ultrasound and CT/MRI, and the tendency for pseudoaneurysms to form and resist spontaneous closure under anticoagulant therapy, the most probable diagnosis is “Pseudoaneurysm in the left calf tendon region, combined with a left Achilles tendon tear.” If there is any remaining diagnostic uncertainty, confirmation by angiography or further ultrasound examination may be considered.
IV. Treatment Plan and Rehabilitation
Treatment Strategy:
1. Interventional Therapy: For larger pseudoaneurysms or those in patients on anticoagulants, ultrasound-guided thrombin injection is commonly used to promote closure. Alternatively, endovascular stenting or embolization may be performed, and surgical ligation is considered when necessary.
2. Management of the Achilles Tendon: Depending on the extent of the tear, surgical repair may be needed when there is severe structural disruption and functional loss. If the tear is minor, conservative treatment with bracing and immobilization followed by rehabilitation may be considered.
3. Prevention of Complications: After surgery or interventional treatment, the patient should avoid extensive weight-bearing and vigorous activities to reduce the risk of pseudoaneurysm re-rupture. Monitoring of hematological parameters is also essential to prevent thrombosis or bleeding complications.
Rehabilitation/Exercise Prescription Suggestions (FITT-VP Principle):
1. Early Stage (Acute Phase): Focus on immobilization and protection, avoiding excessive stretching of the Achilles tendon or high tension to the posterior calf. Under the guidance of a physician or physical therapist, perform gentle ankle joint exercises (e.g., ankle pump) daily for about 5 minutes, 3–4 times per day, at low intensity (range-of-motion exercises without added resistance).
2. Intermediate Stage (Recovery Phase): Once the pseudoaneurysm is stable and the Achilles tendon is partially healed, gradually introduce eccentric-concentric strengthening and proprioception exercises, such as seated calf stretches or elastic band-assisted ankle exercises. Maintain a moderate load intensity, about 15–20 minutes per session, 3 times per week.
3. Late Stage (Reinforcement Phase): After confirming pseudoaneurysm closure and significant recovery of Achilles tendon function, under specialized rehabilitation guidance, progressively add calf muscle strength exercises (e.g., toe raises, balance training) within the patient’s tolerance. Low-impact aerobic activities (such as on an elliptical trainer) can be introduced, 20–30 minutes each session, 3–5 times per week, with individualized adjustments based on cardiovascular status.
4. Progression and Monitoring: Reassess every 2–4 weeks to evaluate local pain, swelling, and strength recovery, and adjust exercise frequency and intensity accordingly. Pay close attention to cardiac and bleeding risks (due to the patient’s anticoagulant therapy) to ensure safety.
Disclaimer
This report provides a reference analysis based on the available clinical and imaging data and does not replace in-person consultation or professional medical advice. In case of any questions or changes in condition, please seek medical attention promptly and follow professional guidance.
Human Doctor Final Diagnosis
Pseudoaneurysm of left posterior tibial artery associated with Achilles tendon tear