Streptococcus anginosus Spondylodiscitis due to intestinal perforation



Clinical History
Female patient, 81-year-old, admitted 4 days previously with community-acquired pneumonia (CAP), on oxygen therapy and intravenous antibiotics. C-reactive protein (CRP) 229.5mg/L, without leukocytosis. Negative urine cultures. Blood culture with Streptococcus anginosus. An ENT consultation excluded oropharyngeal tract abnormalities. She progressed to septic shock with multiorganic dysfunction. A Computed Tomography (CT) was performed.
Imaging Findings
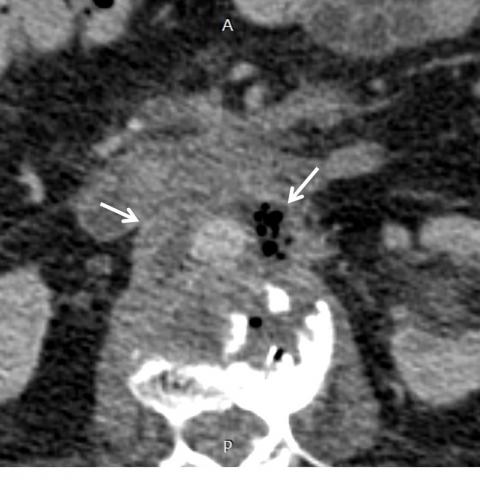
Abdominal and pelvic CT depicted a duodenal neoformative thickening (third portion) and parietal discontinuity, suggesting rupture, confirmed by a subsequent CT with oral contrast (Fig. 1). A fistulous tract, opacified by the oral contrast, lead to a paravertebral collection (L2-L4), with gas, measuring 70mm of maximum diameter, surrounding the infrarenal aorta (Fig. 2). We could also see the oral contrast extending to the intervertebral spaces and anterior epidural space/medullary canal. There were signs of previous vertebroplasty at L2-L3 (Fig. 3).
Peri-pancreatic lymphadenopathy and moderate free fluid were noted (Fig. 4).
There was also an unremarkable bilateral pleural effusion and global cardiomegaly (Fig. 5). No parenchymal consolidations.
The intraoperative appearance was compatible with the imaging findings, with a petrous neoformative mass in the duodenum, with a paravertebral abscess and fistulisation to the lumbar spine. Biopsy was not performed due to haemorrhagic risk. A gastrojejunostomy/duodenojejunostomy were performed. The patient died 10 days after surgery.
Discussion
Spondylodiscitis refers to an infection of the intervertebral discs and vertebral bodies, with high morbidity and mortality. Immunosuppression, diabetes, alcoholism, drug addiction, recent surgical history and spinal trauma are the main risk factors. [1]
The infection can reach the spine by multiple arteries (vertebral or lumbar arteries), veins (Batson venous plexus), by contiguity (secondary to an adjacent abscess) or direct inoculation (accidental or iatrogenic). [2]
Blood cultures are essential but not sufficient in 50 to 75% of the cases and a biopsy is recommended. [1, 4]
The most frequent pyogenic organisms involved are Staphylococcus aureus (60% of cases) and Enterobacter species (30%). [1]
The Streptococcus anginosus (formerly Streptococcus milleri), which was found on our patient’s blood cultures, belongs to the anginosus group, that usually exist inside the paranasal sinuses, oropharynx, gastrointestinal and vaginal tract. [3]
Due to this, we first excluded an ORL origin to the infection by an ENT. The following abdominopelvic CT revealed a neoformative duodenal mass with a fistulous tract to the intervertebral spaces as the cause of the spondylodiscitis and the haematogeneous infection.
CT plays an important role in these cases, allowing evaluation of the intervertebral disc, and characterises epidural involvement (epiduritis/epidural abscess), which may lead to compression of the dural sac and nerve roots. [5] When accompanied by gas at the intervertebral spaces, iatrogenesis by recent interventions or a fistulous tract should be considered, as occurred in our case.
Conventional radiography is insensitive for the first 2-4 weeks.
MRI is the imaging of choice for evaluation, depicting inflammation of the vertebral endplates and peri-vertebral/epidural soft tissues, with focal hyperintensity of the intervertebral disc in T2-weighted image (WI), and a variable enhancement in T1-WI post-contrast. Due to the rapidly progressive course, we were not able to perform an MRI in our patient.
Treatment of choice is intravenous antibiotics accordingly to the pathogen sensitivity. Surgical intervention may be required (in cases secondary to other conditions). The follow-up depends on the clinical response: if good response, X-rays may suffice. MRI is required if a complication is suspected. Systematic MRI is not necessary (no correlation with the clinical improvement). [6]
The radiologist plays an important role in making the diagnosis of spondylodiscitis and determining the source of infection, namely in rarer cases of abscess contiguity.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Streptococcus anginosus spondylodiscitis due to intestinal perforation
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Abdominal and Pelvic CT


Abdominal and Pelvic CT

Sagittal reconstruction



Abdominal and Pelvic CT


Chest CT

Medical Analysis Report
I. Imaging Findings
According to the provided abdominal and spinal CT images, abnormal density can be observed in certain lumbar vertebral bodies (mainly in or around T12 to L1) and adjacent intervertebral spaces. Irregular destruction is noted along the edges of the vertebral bodies and intervertebral discs, and local gas density shadows are present (suggesting infection or fistula formation). Meanwhile, in the abdominal view, there appears to be a neoplastic-like lesion in the duodenum, with increased soft tissue density that extends into the prevertebral space, indicating a possible fistulous tract. Paravertebral soft tissue and the spinal canal also show signs of inflammation or abscess (e.g., soft tissue swelling, increased density, local gas shadows), which helps delineate the scope and route of infection.
II. Potential Diagnoses
-
Vertebral and Intervertebral Disc Infection (Spondylitis/Discitis, or Pyogenic Spinal Inflammation—Spondylitis/Discitis/Abscess)
Reason: CT imaging reveals destructive changes in the vertebral bodies and intervertebral discs along with surrounding purulent or inflammatory findings, and blood culture identified Streptococcus anginosus, suggesting hematogenous or contiguous infection involving the spine. -
Direct Spread from an Adjacent Infectious Source (Duodenal Lesion or Abscess Extending to the Vertebra)
Reason: The abdominal CT shows a suspicious duodenal lesion and possible fistulous tract, correlating with vertebral involvement, indicating that a gastrointestinal infection (or a tumor with infection) may have directly spread to the intervertebral space. -
Secondary Abscess, such as Psoas Abscess or Paravertebral Abscess
Reason: Such an abscess may be secondary to gastrointestinal or vertebral pathology. CT findings of paravertebral soft tissue swelling and gas should prompt consideration of this possibility.
III. Most Likely Final Diagnosis
Taking into account the patient’s advanced age, severe infection signs during hospitalization (significantly elevated CRP, blood culture positive for Streptococcus anginosus), and imaging that displays a duodenal lesion or mass adjacent to and communicating with the intervertebral space, the most likely diagnosis is:
“Duodenal neoplasm (or ulcerative lesion) with spinal infection (spondylitis/discitis), forming a fistula and causing paravertebral/spinal canal infection or abscess,” i.e. “contiguous spinal infection (spondylitis/discitis) from a gastrointestinal lesion.”
Due to indistinct lesion boundaries, fistula formation, and multi-organ dysfunction, this condition constitutes a severe infectious disease requiring collaborative management by multiple departments (Gastroenterology, Orthopedics, Infectious Diseases, and Radiology) for a comprehensive evaluation. If further clarification of the lesion is necessary, endoscopic examination and/or biopsy of the duodenal mass may be performed to determine its pathology, while a vertebral biopsy could be considered if needed.
IV. Treatment Plan & Rehabilitation
- Treatment Plan
- Antimicrobial Therapy: Based on blood culture findings and drug sensitivity, choose appropriate antibiotics (e.g., penicillin-based or other medications effective against Streptococcus anginosus) with sufficient dosage and prolonged IV application (typically at least 6 weeks). Monitor inflammatory indicators and blood cultures closely.
- Control of the Primary Lesion: If the duodenal lesion proves malignant, involves severe ulcerative changes, or forms an abscess, further evaluation by Gastroenterology or GI Surgery is necessary. Surgical resection or drainage may be indicated. With fistula formation and vertebral abscess, Orthopedic or Surgical intervention for abscess drainage or operative management might be warranted.
- Supportive Care: Provide symptomatic treatment, including maintenance of fluid and electrolyte balance, nutritional support, correction of anemia, and cardiopulmonary support as required. Especially in elderly patients, pay attention to multi-organ function to prevent organ failure.
- Individualized Surgical Indications: In the event of significant spinal instability, neurological compression, large abscesses, or failure of conservative management, consider surgical decompression, debridement, and stabilization as necessary.
- Rehabilitation Plan & Exercise Prescription
After initial infection control and stabilization of underlying conditions, an individualized rehabilitation program should be instituted. For elderly patients, exercises must be introduced cautiously within a safe margin.
- Frequency: Aim for 3-5 sessions per week, gradually increasing based on patient tolerance.
- Intensity: Begin with very light to light intensity (e.g., sitting by the bedside, bed-based joint exercises). As tolerance increases, consider moving to moderate intensity, such as indoor walking or short walks using assistive devices.
- Time: Initially, allow 10-15 minutes of total exercise daily in divided intervals. As recovery progresses, extend to 20-30 minutes per day.
- Type: Favor low-impact activities that help maintain muscle strength and joint flexibility, for instance seated or upright walking, light resistance exercises (with bands or light dumbbells), as well as breathing and simple bed exercises.
- Progression: With improvement in inflammation and pain relief, patients can incrementally increase loading or walking duration, and focus on strengthening back and core muscles (e.g., gentle supine leg lifts or supported standing). Proceed gradually.
- Special Considerations: As the patient is elderly with multi-organ comorbidities, guard against hypotension, excessive cardiopulmonary stress, and fracture risk during exercise. Rehabilitation should be supervised by professionals or assisted by family members, with appropriate use of walking aids or canes for safety.
V. Disclaimer
This report is based on the current clinical and imaging data as a reference, and does not replace face-to-face medical consultation or professional medical advice. Patients should follow recommendations from specialists or multidisciplinary teams. In the event of symptom exacerbation or any urgent situations, seek immediate medical attention.
Human Doctor Final Diagnosis
Streptococcus anginosus spondylodiscitis due to intestinal perforation