Coracoid processes fracture associated with anterior shoulder dislocation


Clinical History
An 18-year-old male presented to the emergency department after an epileptic seizure with no memory of the episode. On physical examination, pain and left shoulder deformity were present.
Imaging Findings
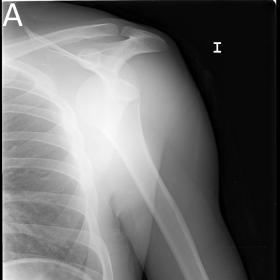
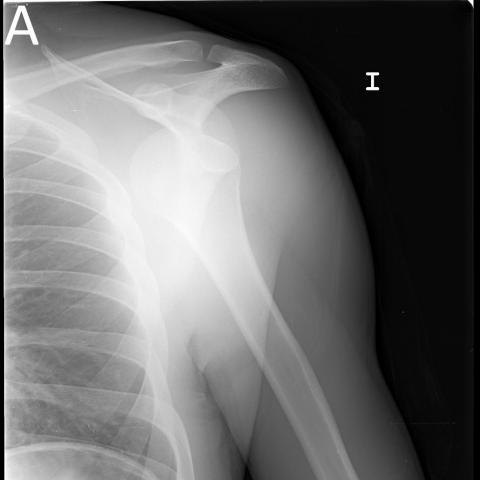
Plain radiographs on anteroposterior and scapular “Y” view were performed, demonstrating anterior-inferior glenohumeral dislocation (Figure 1A and 1B). The dislocation was correctly reduced and confirmed with a new radiographic study.
Due to persistent and notable pain three weeks after the acute episode, shoulder magnetic resonance imaging (MRI) was performed. This exam demonstrated a wedge-shaped depression along the postero-lateral aspect of the humerus (Hill-Sachs lesion) and a labral Bankart lesion with no osseous involvement and without signs of rotator cuff or neurovascular structures involvement (Figure 2 A and B).
Incidentally, a marked hyperintensity on liquid-sensitive sequences and a fracture line on the coracoid process were noted (Figure 2 C and D). No pathological findings were found on the short head of the biceps brachii or coracobrachialis muscles.
A shoulder CT was performed to accurately define the fracture. Findings were compatible with non-displaced Ogawa type II fracture anterior to the coracoclavicular ligaments (Figure 3).
Discussion
Coracoid fractures are uncommon, and when present tend to occur in association with glenohumeral dislocation. This association accounts for only 2% of injuries around the shoulder girdle.
This fracture occurs mainly due to two mechanisms. One is the avulsion from a violent contraction of the muscles attached (pectoralis minor, and conjoined tendon of the biceps and coracobrachialis muscles), and the second mechanism involves the direct impact of the dislocated humeral head against the coracoid process, being the last one the most frequent. [1,2].
Coracoid fracture can be easily missed on standard shoulder radiography (AP projection and internally and externally rotated projections). To detect these fractures, it is helpful to obtain complimentary views such as axillary or “Y” views.
The axillary view provides more information about the shoulder than any other single projection [3]. It is the only view in which minimally displaced fractures of the coracoid process of the scapula, cortical fractures of the anterior or posterior surfaces of the humeral head, posterior dislocation of the humerus, and direction of angulation of proximal humeral fracture fragments can be conclusively demonstrated [4] After reduction this projection is useful to assess for Hill-Sachs fractures and associated scapular fractures.
Nevertheless, axillary projection can be hard to obtain during an episode of glenohumeral dislocation due to the impossibility to perform 90º abduction. Because of this, a modified axillary radiograph was described by Senna et al. [3), with no more than 30º of shoulder abduction.
According to the Ogawa classification, this fracture corresponds a type II without compromise of coracoclavicular ligaments [5]. This fracture is less unstable than type I and usually resolves well when conservative treatment is taken on [4]. Surgical management is considered for fractures with intraarticular extension or more than 1 cm of displacement between fragments [6].
Differential Diagnosis List
Final Diagnosis
Coracoid process fracture in an episode of anterior glenohumeral dislocation
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures









1. Imaging Findings
On the anteroposterior (AP) X-ray of the shoulder (Figures A and B), there is an interruption in the continuity of the bony structure or an abnormal morphology in the coracoid process region beneath the acromion, suggesting the possibility of a coracoid process fracture.
On MRI (Figures A–D), a signal disruption or increased signal can be seen at the coracoid process, accompanied by local soft tissue swelling. No significant tear is observed in the surrounding joint capsule or tendons (such as the biceps tendon), though mild edema is present. Certain slices show a slight injury signal in the humeral head (potential “Hill-Sachs”-like change), which requires clinical correlation to determine whether there is a partial shoulder dislocation or an impact-related associated bone contusion.
CT (3D reconstruction Figures C and D) clearly demonstrates the fracture line of the coracoid process, consistent with the proximal and distal demarcation described in Ogawa’s classification. No obvious large-scale displacement is noted between the fracture segments, nor is there any significant involvement of the attachment site between the coracoid process and the coracoclavicular ligaments.
2. Differential Diagnosis
- Coracoid Process Fracture: Based on the imaging findings and clinical symptoms, a coracoid process fracture is a primary consideration. It may be caused by forceful muscle contraction or an impact from the humeral head during shoulder dislocation.
- Acromial or Glenoid Rim Fracture: If trauma or dislocation is present, an acromial or glenoid rim fracture should be considered; however, imaging does not reveal any clear fracture lines in these areas.
- Shoulder Dislocation with Associated Bony Lesions (e.g., Hill-Sachs Lesion): The MRI signal suggests a localized humeral head injury that could be associated with shoulder dislocation. However, current imaging does not clearly indicate a definite dislocation.
Considering the patient’s history of trauma (or forceful muscle contractions such as those occurring during seizures) and the radiographic features, a coracoid process fracture is the most consistent finding.
3. Final Diagnosis
Taking into account the patient’s age, clinical presentation (intense muscle contractions due to seizure episodes), and the multiplanar imaging findings (X-ray, MRI, and CT) indicating a coracoid process fracture, the most likely diagnosis is Coracoid Process Fracture (Ogawa Type II), with no significant involvement of the coracoclavicular ligament attachment.
4. Treatment Plan and Rehabilitation
Treatment Strategies:
1. Conservative Treatment: For Ogawa Type II coracoid fractures with minimal displacement (< 1 cm), conservative therapy is typically preferred. This includes using a shoulder brace or sling for a period (approximately 3–6 weeks) to reduce local stress and movement, aiming to prevent secondary injury.
2. Surgical Treatment: If there is significant displacement (> 1 cm) or severe involvement of the articular surface, surgical fixation may be necessary to ensure long-term shoulder stability and functional recovery.
Rehabilitation/Exercise Prescription Recommendations (FITT-VP Principle):
1. Early Phase (Immobilization, approximately 3–6 weeks):
• Primarily maintain relative immobilization of the affected shoulder, avoiding excessive force and traction.
• Perform gentle passive shoulder exercises (e.g., pendulum exercises) if they do not compromise fracture healing, in order to preserve joint mobility and prevent adhesions.
• Frequency (F): 1–2 sessions per day; Time (T): 5–10 minutes per session; Intensity (I): extremely light or within a pain-free range.
2. Middle Phase (After Removing Immobilization to about 8–12 weeks):
• Once the fracture is largely healed and stable, gradually increase active range of motion and strengthen the muscles around the shoulder (e.g., light resistance band exercises, shoulder abduction and adduction training).
• Frequency (F): 3–4 sessions per week; Time (T): 20–30 minutes per session; Intensity (I): light to moderate resistance, progressing gradually, ensuring no significant pain.
• Type of Exercise (T): Active range-of-motion exercises, isometric contractions, and resistance band work.
• In this phase, monitor pain and swelling carefully, and adjust volume and progression (V, P) accordingly.
3. Late Phase (After 3 months):
• Gradually incorporate functional training, such as internal and external rotation, overhead movements, and daily activities (e.g., lifting objects).
• Progressively return to normal exercise intensity; for those resuming sports (e.g., throwing), first undertake specialized stability and coordination training.
• Frequency and duration can be increased according to the patient’s tolerance. For individuals with weaker bone quality or poor shoulder stability, a longer preparatory period is recommended.
Disclaimer
This report is provided as a reference based on available history and imaging data and cannot substitute for in-person consultation or professional medical advice. The specific diagnosis, surgical procedures, and rehabilitation plan should be determined after a thorough clinical evaluation and any additional necessary tests.
Human Doctor Final Diagnosis
Coracoid process fracture in an episode of anterior glenohumeral dislocation