Large primary lipoma arborescens of the knee



Clinical History
A 44-year-old male patient presented with chronic swelling along the anterior aspect of the right knee for at least 5 or 6 years. He had a history of trauma 10 years back. There was no associated pain, but a decreased range of motion was found on physical examination.
Imaging Findings
The X-ray showed right knee swelling, involving mainly the suprapatellar region with decreased opacity and lateral displacement of the patella (Figures 1a and 1b).
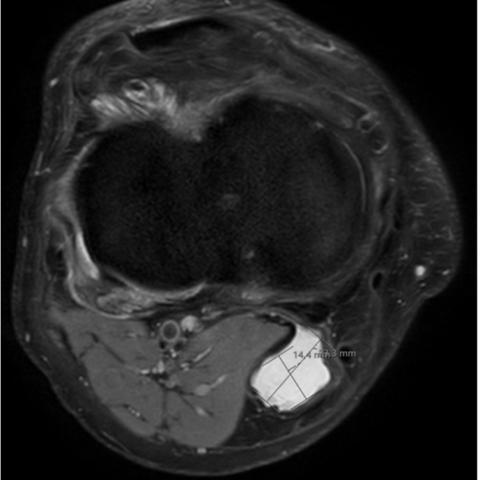
The MRI revealed moderate joint effusion with marked distension of the joint capsule due to the presence of diffuse vegetations with high T1 signal (Figure 2), low signal on T2* (Figure 3) and high PD signal that becomes low signal on fat-suppressed (FS) sequences (Figures 4a, 4b, 4c and 4d). There is also an extension of the effusion into a Baker’s cyst measuring approximately 63 x 23 x 14 mm (Figures 5a and 5b).
Discussion
Background
Lipoma arborescens is a rare, benign intra-articular lesion characterised by villous proliferation of the synovial membrane and replacement of the subsynovial tissue by mature fat cells. This condition typically affects the knee joint but can occur in other joints, such as the shoulder, elbow, wrist, hip, and ankle [1,2].
Pathophysiology
The condition involves the transformation of normal synovial tissue into hypertrophied villi with significant fat deposition. The exact cause of lipoma arborescens is unclear, but it may be linked to chronic inflammation, trauma, or degenerative joint disease [2,3]. Recent studies identify two forms: primary and secondary. The secondary form is the most common and is typically associated with degenerative joint pathology or meniscopathy, often occurring in older patients. In contrast, primary lipoma arborescens, characterised by exuberant hypertrophied villi, typically occurs in younger adults without other joint changes [4]. In our case, despite a history of knee trauma, there were no signs of old fractures or degenerative arthritis. The extensive hypertrophied villi suggest a primary pathology.
Clinical Perspective
Patients often present with chronic joint swelling, variable arthralgia, and decreased range of motion. The symptoms can mimic those of other joint diseases, such as arthritis or synovitis [5,6].
Imaging Perspective
Plain radiograph – Sometimes can detect fatty lucencies within a soft tissue lesion, but they are usually overshadowed by the associated effusion. Degenerative changes are often present, while osseous erosions are rare [2].
Ultrasound – Typically shows a joint effusion with echogenic “frond-like” projections.
CT – It reveals a low-density intra-articular mass, indicating fat, with minimal or no enhancement [3].
MRI – MRI is the most effective imaging modality for diagnosing lipoma arborescens. It shows characteristic features such as:
- High signal intensity on T1-weighted images due to the presence of fat.
- Decreased signal on fat-suppressed sequences, confirming the fatty nature of the lesion.
- Villous projections extending into the joint space, resembling a “frond-like” or “tree-like” appearance [1,2,7].
Outcome
Conservative Management – Initial treatment may include anti-inflammatory medications and physical therapy to manage symptoms.
Surgical Intervention – Arthroscopic synovectomy or open synovectomy is often required to remove the fatty villous proliferation. This is particularly necessary if the condition causes significant symptoms or functional impairment.
Prognosis – After surgical treatment, it is generally good, with most patients experiencing relief from symptoms. Recurrence is uncommon [5].
Take Home Message
Lipoma arborescens is a rare, benign intra-articular condition characterised by fatty villous proliferation within the synovial membrane, typically affecting the knee. It presents with chronic joint swelling and possible pain, often resembling arthritis. MRI is the diagnostic gold standard, revealing high T1 signal and low signal on fat-suppressed sequences. Surgical removal is often necessary for lasting relief.
Differential Diagnosis List
Final Diagnosis
Lipoma arborescens
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
X-rays


MRI Coronal T1

MRI Coronal T2

MRI PD




MRI PD

Medical Imaging Analysis Report
I. Imaging Findings
Based on the provided X-ray and MRI images, multiple “leaf-like” or “flocculent” soft tissue proliferative shadows are observed within the right knee joint space, characterized as follows:
- X-ray: The joint surface morphology is generally normal, with no obvious bone destruction or signs of fracture. There is an increased soft tissue shadow, suggesting abnormal proliferation or effusion in the joint cavity, though the fat component is difficult to identify accurately.
- MRI: On T1-weighted images, the lesion shows high signal intensity, and the signal is markedly reduced on fat suppression sequences, indicating that the lesion mainly consists of fatty tissue. “Cluster-like” or “finger-like” protrusions can be seen, exhibiting a “branch-like” proliferation consistent with the typical presentation of fatty villous proliferation. There is no significant destruction or deformation of the articular cartilage, meniscus, or bone structure.
The overall imaging characteristics strongly suggest an intra-articular fatty villous proliferative lesion, with no obvious erosion or significant bone abnormality adjacent to it.
II. Possible Diagnoses
- Lipoma arborescens
Features: An intra-articular fatty lesion commonly found in the knee joint. On MRI, it appears with high signal on T1-weighted images and a marked signal reduction on fat-suppressed sequences, presenting as a “villous” or “branch-like” protrusion. - Synovial chondromatosis
Features: Cartilaginous or calcified nodules in the joint or within the synovium. It may present with knee swelling and “joint mice.” Classic calcific densities are often visible on X-ray or CT scans. - Pigmented Villonodular Synovitis (PVNS)
Features: Proliferation of the synovium with possible joint effusion and synovial thickening. On T2-weighted images, some lesions show low signal intensity due to hemosiderin deposition. The lesion is not primarily composed of fatty tissue. - Other Inflammatory Synovial Proliferations (e.g., Inflammatory Arthritis)
Features: Synovial thickening due to inflammatory exudates and enhancement, lacking the significant fatty signal characteristics.
Considering the clinical and imaging findings, Lipoma arborescens is the most representative diagnosis.
III. Final Diagnosis
Taking into account the patient’s history of prolonged anterior knee swelling, mild trauma, and MRI findings showing high signal in fatty components with branch-like proliferation, the most likely diagnosis is:
Lipoma arborescens.
If further confirmation is required, arthroscopic biopsy for pathology can be performed to rule out other rare synovial lesions.
IV. Treatment Plan and Rehabilitation Program
1. Conservative Treatment
For patients with milder symptoms, conservative treatment may be considered, including:
- Oral or intra-articular injection of non-steroidal anti-inflammatory drugs (NSAIDs) to reduce synovial inflammatory response.
- Appropriate rest combined with ice therapy to alleviate joint swelling.
2. Surgical Intervention
If joint mobility is significantly limited or swelling persists for a long time, arthroscopic or minimally invasive synovectomy may be considered. The goal is to remove the excessively proliferated fatty synovial tissue, reduce mechanical irritation, and improve range of motion.
3. Rehabilitation and Exercise Prescription
Whether managing the condition conservatively or post-treatment, an individualized and gradual rehabilitation program is essential:
- Frequency: 3–5 times per week, adjusted according to individual tolerance and joint response.
- Intensity: Low to moderate intensity is appropriate, ensuring safety and avoiding excessive joint pain or swelling.
- Type:
- Range of motion exercises: Active flexion and extension under non-weight-bearing conditions, as well as passive stretching to improve knee range of motion.
- Strength training: Quadriceps, hamstrings, etc., using isometric or low-resistance exercises. In the early stages, exercises such as leg raises or straight-leg raises on flat ground can be performed.
- Functional training: Practicing sitting, standing, and walking balance. In later stages, gentle squats may be considered (avoiding excessive load).
- Assisted training: If feasible, water-based exercises (e.g., walking in water) can help reduce joint stress while improving muscle strength.
- Time: Each session should last about 20–30 minutes, with the possibility of gradual increases based on joint tolerance.
- Volume: Aim for at least 60–90 minutes of rehabilitation exercise per week, divided into multiple sessions.
- Progression: As pain subsides and range of motion improves, gradually increase range of motion, resistance, or walking speed. Ensure a step-by-step approach, avoiding sudden increases in load.
For patients with existing joint degeneration or those in the postoperative recovery phase, professional guidance from a rehabilitation therapist or sports medicine specialist is recommended to ensure both safety and effectiveness.
V. Disclaimer
This report is based solely on the provided medical history and imaging information and is intended to offer a preliminary analysis for clinical reference. The actual treatment plan must be tailored to the patient’s comprehensive evaluation and the advice of a qualified physician. If symptoms change or worsen, please seek medical attention promptly.
Human Doctor Final Diagnosis
Lipoma arborescens