Sciatica: A pitfall clinical diagnosis of septic sacroiliitis



Clinical History
A 32-year-old male with a long history of low-intensity intermittent sciatica, conservatively treated, was referred to the radiology department, presenting with a 14-day history of pain in the lower back radiating posteriorly to the left limb and groin. He had been skiing the week before developing the pain but denied any trauma.
Imaging Findings
Although the neurologist recommended lumbar spine MRI based on the history and physical examination, during the initial stages of acquisition, large pelvic collections adjacent to the left sacroiliac joint drew attention. Therefore, the examination was shifted to a pelvic MRI, using the sacroiliac joint protocol.
Pelvic MRI revealed massive inflammatory changes in the left sacroiliac joint: enlarged articular space with fluid effusion; extensive periarticular bone marrow oedema; soft-tissue inflammation seen as inhomogeneous low T1-WI, high T2-WI/PD signal of the adjacent left hip muscles (gluteus muscles, iliac, iliopsoas, piriformis, internal obturator - at origin, superior gemellus - more subtle) and of left erector spinae muscles at insertion; numerous synovial fluid outpouchings arising from anterior, posterior and inferior aspects of sacroiliac joint, dissecting away into the depth of gluteus maximus and medius, piriformis, erector spinae muscles, and iliac muscle. The left sciatic nerve appeared edematous, in contact with the abscess wall within the piriformis muscle.
After contrast administration, enhancement of bone and muscle reactive oedema and thick rim enhancement of fluid outpouchings and collections were noted.
Interestingly, bone marrow oedema of the right aspect of sacrum involved left S2-S4 neural foramina, with inflammatory changes of the nerve roots.
Discussion
Septic arthritis is an inflammatory condition of joints caused by infection with different microorganisms, most frequently bacterias (95%). The sacroiliac joints are a rare location of septic arthritis, accounting for 1-2% of all cases. [1]
Septic sacroiliitis (SSI) can occur from hematogenous spread, direct inoculation secondary to invasive medical procedures and trauma, or by contiguous spread from an adjacent infection process. The commonest etiological agent of SSI is Staphylococcus aureus; others include gram-negative microorganisms or Mycobacterium tuberculosis. [2,3]
As in our case, the heterogeneous and non-specific clinical manifestation of SSI can lead to a delayed diagnosis. Symptoms such as lombogluteal pain (most common), coxofemoral pain, or pelvic pain, to which is added the absence of fever (64,7% of cases), give rise to a diagnostic challenge for the clinician. The biological inflammatory syndrome, although suggestive of SSI, is inconsistent and variable in terms of amplitude. Therefore, the clinical and paraclinical ensemble may be interpreted as lumbar disc herniation, spondylodiscitis, hip pathology, or gynaecological/digestive pathology, leading to a protracted-time to diagnosis, with serious consequences on the patient's outcome. [4,5]
In order to achieve the diagnosis, imaging plays a crucial role.
X-ray is not usually of help, being unremarkable in the early stages. Ultrasound's role may be found in arthrocentesis guidance, although CT-guided procedures are more frequently used, as the sacroiliac joint is hard to reach, and so, its puncture has a high technical difficulty. [2,3]
CT and MRI are the imaging techniques with the highest reliability in diagnosing SSI. CT is able to show signs of inflammation such as widening of the sacroiliac joint, erosions, soft tissue swelling, and abscess formation. However, early abscesses may be easily missed; also CT's incapability to detect subtle bone changes or display bone fluid is well known. [3,6]
MRI has the highest sensitivity in detecting and characterizing in terms of extent and distribution the early inflammatory changes of the sacroiliac joint, such as joint effusion, periarticular bone oedema, soft-tissue swelling; also has a better performance in describing a possible spread of infection to muscle and abscess formation. MRI proves a 50% higher detection rate compared to CT and bone scintigraphy. Consequently, MRI is considered the reference imaging technique in diagnosing SSI. [3,5,7]
SSI is extremely rare a bilateral condition. Unilaterality is not pathognomonic for infectious aetiology, as it may also be seen in spondyloarthropathies, but the first diagnosis to exclude when facing unilateral sacroiliac joint changes on imaging is SSI. [9]
Microbiological analysis of the synovial fluid (usually obtained by CT-guided joint puncture) or positive blood cultures followed by antibiotic-sensitivity testing are important tools contributing to the diagnosis and mandatory requirements for treatment implementation, which is rapid and aggressive intravenous antibiotic therapy according to the implied microorganism. Surgical treatment is indicated in case of lack of response. [1,5]
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Septic sacroiliitis
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Axial PD (1a), axial T2-WI (1b), and coronal T1-WI (1c)



Pre- (2a) and postcontrast (2b) axial T1 FS
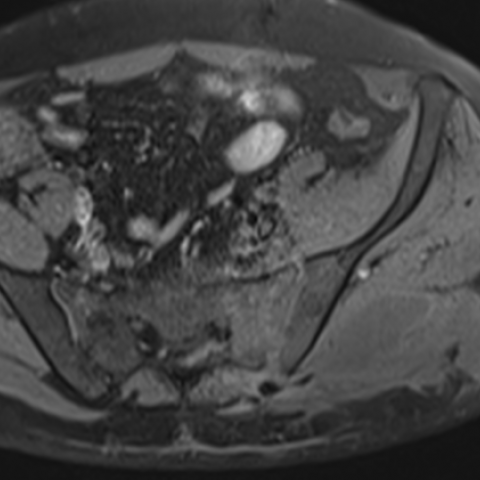

Axial PD

Coronal T2-WI (4a) and sagittal post-contrast T1 FS (4b)


1. Radiological Findings
The patient is a 32-year-old male who presents with lower back pain radiating to the left lower extremity and groin area for approximately two weeks. He has a history of chronic, intermittent sciatica. The current MRI primarily shows the following features:
- Sacroiliac joint changes: The left sacroiliac joint space is irregular, with abnormal signal in the adjacent bone. Bone marrow edema and soft tissue swelling are observed around the joint, showing increased signal on T2WI/fat-suppressed sequences, suggesting local inflammatory changes.
- Possible joint effusion or abscess: Fluid signal is seen around the left sacroiliac joint, with marginal enhancement, indicating possible joint effusion or early abscess formation.
- Involvement of surrounding soft tissue: Slightly high signals can be seen in local muscular and fascial compartments, suggesting inflammatory infiltration or infection spread.
- No obvious fracture: There is no clear disruption of the cortical bone, but mild erosion or destruction may be present in infected bone areas.
2. Potential Diagnosis
Based on the above imaging and clinical presentation, the possible diagnoses include:
- Infectious sacroiliitis (pyogenic sacroiliitis): Common pathogens include Staphylococcus aureus. Findings typically include bone marrow edema around the joint, soft tissue swelling, and even abscess formation within or around the joint. Clinically, patients may present with pain and limited mobility, and some cases may not show significant fever in early stages, leading to misdiagnosis.
- Paraspinal infections (e.g., lumbosacral paravertebral abscess, vertebral osteomyelitis): If the infection spreads to the lumbosacral vertebrae or paravertebral space, epidural or psoas abscesses may occur. However, in this case, the primary involvement is the sacroiliac joint, with less prominent changes in the vertebral bodies and intervertebral discs.
- Ankylosing spondylitis or other spondyloarthropathies: These conditions can involve the sacroiliac joints. However, they often present as chronic, bilateral, or symmetrical lesions with associated back stiffness. A unilateral, asymmetric severe lesion raises suspicion of infection first.
- Hip joint or other pelvic lesions: For example, hip synovitis or pelvic tumors can produce radiation pain similar to that involving the lumbosacral region. However, these can be largely ruled out in this case based on the imaging features.
3. Final Diagnosis
Taking into account the clinical presentation (lumbosacral to groin radiating pain, acute exacerbation, no obvious trauma) and the imaging findings of unilateral sacroiliac joint inflammatory changes, local soft tissue swelling, and possible purulent fluid, the most likely diagnosis is:
Infectious sacroiliitis (pyogenic sacroiliitis).
To confirm, a sacroiliac joint aspiration and culture could be performed, along with hematology tests (white blood cell count, CRP, ESR, etc.) to identify the pathogen and conduct drug susceptibility testing.
4. Treatment Plan and Rehabilitation
4.1 Treatment Strategy
- Intravenous antibiotic therapy: After obtaining microbiological results and drug sensitivity tests, use appropriate antibiotics for a sufficient duration. For Staphylococcus aureus, anti-staphylococcal penicillins or cephalosporins are commonly chosen.
- Joint aspiration and drainage/catheter placement: If an abscess or purulent collection is present, image-guided drainage can be performed to relieve local symptoms and reduce the spread of infection.
- Surgical intervention: If conservative management and antibiotic therapy fail or infection control becomes difficult, surgical debridement may be necessary.
- Symptomatic and supportive care: This includes pain relief, reduction of swelling, rest, and support for overall nutritional status.
4.2 Rehabilitation and Exercise Prescription
After the acute infection or fever subsides, a gradual exercise and functional training program can be introduced, following the FITT-VP principle:
- Type of exercise: Initially focus on joint mobilization exercises and stretching activities, combined with gentle core stabilization exercises (e.g., planks, small-range trunk rotations).
- Frequency: 3-5 sessions per week, adjusted according to the patient’s recovery.
- Intensity: Begin with low intensity, ensuring it does not provoke significant pain or fatigue, then increase steadily based on individual tolerance.
- Time: Start with 10-15 minutes per session, progressively extending to around 30 minutes. Perform warm-up before exercise.
- Progression: Once pain and inflammation are well controlled, add weight-bearing activities and further joint functional training. If discomfort arises, adjust or pause accordingly.
- Volume and Pattern: Increase the variety of exercises and sets gradually, avoiding abrupt increases in workload.
Pay close attention to stability and posture control around the affected joint in the early stages of rehabilitation. If osteoporosis or other systemic issues are present, exercise caution and consider professional guidance from a rehabilitation therapist or physical therapist.
5. Disclaimer
This report is based on imaging and existing clinical information and is for reference only. It cannot replace in-person consultation or the diagnosis and treatment advice of a professional physician. If you have any questions or if your condition changes, please seek medical attention promptly and follow your clinician’s guidance.
Human Doctor Final Diagnosis
Septic sacroiliitis