Lymphatic malformation of the dorsal scapular neurovascular bundle


Clinical History
A 35-year-old male presented with chronic right interscapular pain associated with mild scapular dyskinesia. The pain was refractory to conservative treatment and due to a history of an effort-induced thrombosis of his right subclavian vein, an atypical thoracic outlet syndrome with involvement of the dorsal scapular nerve was suspected.
Imaging Findings
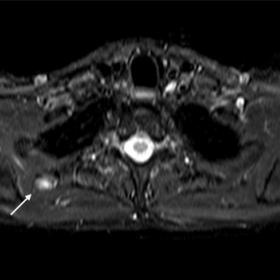
MR imaging of the scapular area revealed a 1 x 1 x 1.5 cm circumscribed mass which demonstrated high-intensity signal in fluid sensitive sequences (STIR) (Fig. 1) (Fig. 2). The mass was located adjacent to the dorsal scapular neurovascular bundle ventrally to the insertion of the minor rhomboid in a space normally occupied by fat. The lesion showed mild but evident contrast enhancement and a fascicular cross-sectional structure in the axial images (Fig. 3). Mild muscle asymmetry was noted with slight atrophy of the right major rhomboid muscle. A certain diagnosis could not be established and an ultrasound-guided lidocaine injection was performed to evaluate possible response or improvement of the symptoms. The injection aggravated the symptoms for a week which prompted the surgical exploration of the area and the excision of the lesion on the suspicion of compression of the dorsal scapular nerve. A 1 cm microcystic lymphatic malformation that surrounded the nerve was excised. The patient’s symptoms remained unchanged.
Discussion
Interscapular pain is a common clinical issue with a varying aetiology including discogenic pain, facet syndrome, myofascial pain syndrome (MPS) of upper back muscles, and back strain in the dorsal region. The involvement of the dorsal scapular nerve has been debated and an entrapment of this nerve has been postulated [1] as one of the causes. The most common anatomic location of entrapment is considered the middle scalene [2] which has been viewed as an atypical form of thoracic outlet syndrome [3], though its existence is still controversial.
The atypical presentation of dorsal scapular nerve entrapment pertains to the absence of significant neurogenic symptoms in the upper extremity with symptoms and signs mostly located in the interscapular area or the paraspinal area. This spectrum includes varying levels of pain intensity and character along a portion of or its entire pathway of the nerve and ranges from complete function to complete atrophy of the muscles it innervates[4].
In the majority of cases, imaging investigation of interscapular pain is limited to MR examination of the cervical, thoracic spine or glenohumeral joint. Imaging of the periscapular area is seldom performed and is mostly focused on suspected scapulothoracic bursitis. The oval fat-containing space that is demarcated by the minor rhomboid, the anterior serratus and the caudal part of levator scapula and contains the dorsal scapular vessels is clearly visible when the patient is examined with the arms parallel to the torso (Fig. 4). This space is obliterated when the patient raises their arms above their head, e.g for most CT examinations. The presence of a mass lesion in this area can be misleading in a patient with interscapular symptoms.
The lesion which has not been described previously in the radiologic or anatomic literature is a lymphatic malformation adjacent to the dorsal scapular neurovascular bundle with a rather high prevalence and varying size in this particular anatomic location to the authors’ experience.
Take-Home Message
Radiologists should be aware of the dorsal scapular lymphangioma and should dismiss it as an incidental finding with no clinical significance, especially in patients that undergo imaging for non-specific chronic unresolving periscapular or interscapular symptoms. The size of the lesion can vary and can mislead the treating physician into an unnecessary and risky surgery that could damage the dorsal scapular nerve or the closely coursing spinal accessory nerve.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Lymphatic malformation of the dorsal scapular neurovascular bundle
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures





1. Radiological Findings
Based on the provided MRI images, a well-defined soft tissue lesion is observed in the medial side of the right scapula (i.e., between the rhomboid muscle, serratus anterior, and the posterior part of the levator scapulae). On conventional T1-weighted sequences, the lesion appears as hypo- or iso-intense; on T2-weighted or fat-suppressed sequences, it displays hyperintense or mixed signals, suggesting the presence of fluid or lymphatic-like components. There is no obvious bone destruction or strong enhancement, and the lesion is located near the route of the dorsal scapular nerve and the accompanying vascular bundle.
Meanwhile, mild muscle morphological abnormalities are noted in the medial scapular area on the right side. In certain areas, the muscle bundles appear slightly disorganized, indicating mild scapular positional or kinematic abnormalities (such as scapular instability or scapular dyskinesis). No significant spondylolisthesis, vertebral fracture, or evident soft tissue mass compressing the spinal canal is observed.
2. Potential Diagnoses
-
Dorsal Scapular Nerve Entrapment:
Given the patient’s chronic medial scapular pain and mild scapular movement dysfunction, compression of the dorsal scapular nerve can lead to dysfunction of the rhomboid or levator scapulae, clinically presenting as discomfort and achy pain in the scapular region. In light of the imaging findings, if a lymphatic lesion or scar tissue is located near the nerve bundle, it may be contributing to an atypical form of thoracic outlet syndrome.
-
Lymphatic Malformation (Lymphangioma):
A fluid-containing, well-demarcated lesion in this area without prominent enhancement suggests a lymphatic malformation (including lymphangioma or a lymphatic cyst). Although “dorsal scapular lymphangioma” is uncommon, literature indicates that when present, it often manifests as a benign space-occupying lesion.
-
Other Cystic Soft Tissue Lesions:
Lesions such as scapulothoracic bursitis or cystic tumors can exhibit similar imaging characteristics, but they often present with marked inflammatory or pain symptoms. Based on current case presentations, this possibility is relatively lower.
-
Muscular or Tendon Lesions:
Conditions such as localized fibromatosis or fibrolipoma may be considered, but given the distinct fluid-like signals seen on MRI, these diagnoses are less likely.
3. Final Diagnosis
Considering the patient’s clinical symptoms (chronic medial scapular pain, scapular instability) and imaging findings (well-defined lesion with fluid or lymphatic-like signals, located near the dorsal scapular nerve and vessels), the most likely diagnosis is:
“Right-sided lymphatic malformation (dorsal scapular lymphangioma) adjacent to the dorsal scapular nerve, with/possible dorsal scapular nerve compression.”
In most cases, such lymphatic malformations may be incidental and clinically insignificant. If there are no significant nerve symptoms or muscle atrophy, surgical intervention is generally not required. However, after ruling out other causes of chronic pain, its relationship to nerve compression may be considered.
4. Treatment Plan and Rehabilitation
(1) Conservative Treatment:
- As the patient’s pain is chronic and there is no significant neurological deficit, continued regular physical therapy and rehabilitation exercises are recommended. These include scapular stabilization exercises, posture correction, and strength training.
- Non-steroidal anti-inflammatory drugs (NSAIDs) or local heat application and massage can be used as appropriate to relieve pain.
(2) Surgical Consideration:
- Surgical intervention may be evaluated if the lymphatic malformation enlarges significantly or causes clear nerve compression symptoms (e.g., persistent severe pain, marked muscle weakness, or muscle atrophy).
- Prior to surgery, thorough neurophysiological testing and/or ultrasound-guided tissue evaluation should be performed to confirm the lesion’s exact impact on the nerve and to avoid unnecessary risks.
(3) Rehabilitation/Exercise Prescription (FITT-VP Principle):
- Frequency (F): Perform rehabilitation exercises targeting the scapula and upper back 3–4 times per week; if symptoms are mild, it can be increased to 5 times per week.
- Intensity (I): Start with low-intensity strength training (e.g., light resistance bands or low-weight dumbbells) and gradually increase resistance.
- Time (T): Each session should last about 20–30 minutes, including warm-up, core exercises, and scapular strengthening.
- Type (T): Focus on scapular stabilization exercises (seated row, bent-over row, rear delt fly on a butterfly machine with light load) and posture correction (such as shoulder shrug exercises, scapular circles, etc.).
- Volume & Progression (VP): Gradually increase load based on pain and fatigue levels. If the patient can maintain proper form without discomfort at the current resistance or during a specific movement, a slight increase in resistance or repetitions can be considered every 2–4 weeks.
During the rehabilitation process, closely monitor the patient’s pain response and joint range of motion. If there is notable sharp pain or numbness, re-examination and adjustment of exercise intensity should be carried out promptly.
Disclaimer
This report is a comprehensive medical analysis based on the existing medical history and imaging data. It is for reference only and cannot replace a face-to-face diagnosis or treatment recommendation from a clinical physician. If you experience discomfort or changes in your condition, please consult a professional doctor in person for further medical evaluation.
Human Doctor Final Diagnosis
Lymphatic malformation of the dorsal scapular neurovascular bundle