


A 53-years-old male was admitted to the orthopaedic consultation complaining of pain and paresthesias in the right foot. At the objective exam, a small mass was detected in the first interdigital space of the right foot, without cutaneous lesions. An ultrasound (US) was first done, and then a magnetic resonance imaging (MRI).
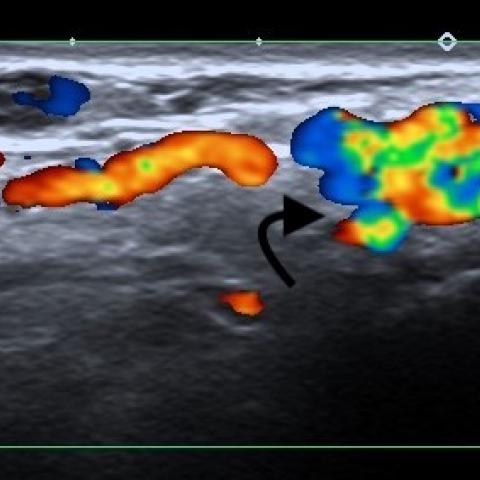
The ultrasound of the first interdigital space of the right foot showed, in the dorsal region, a crooked hypoechogenic lesion, in the plane of the metatarsal heads (Fig. 1). This lesion had codification on colour Doppler with aliasing, near the dependence of the dorsal metatarsal arteries of the Hallux (Fig. 2). In the spectral Doppler is possible to detect in the lesion a low resistance arterial flow, with a high-flow velocity – the maxim of 274 cm/s (Fig. 3).
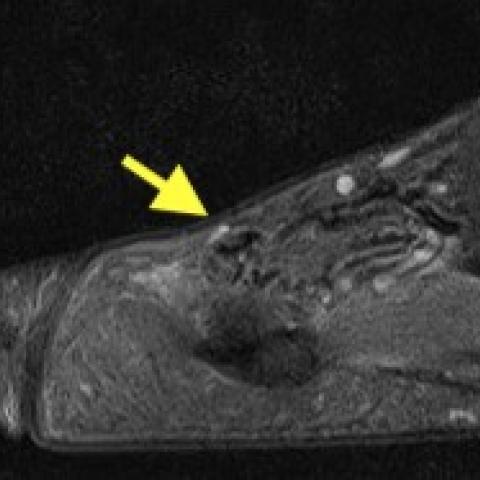
In the MRI, the lesion presented as an oval mass localized in the soft tissue of the dorsal aspect of the first interdigital space, with hypointensity in T1 and multiple small linear structures (“nidus”) in the central of the lesion (Fig. 4). We can also detect areas of the signal void in the nidus, representing the high-flow vascularization (Fig. 5). The T1 post gadolinium sequences showed a venous enhancement to the dorsal and plantar aspects of the interdigital space (Fig. 6).
Vascular malformations of the extremities constitute some of the most difficult diagnostic and therapeutic challenges. Some classifications had been done to try to clarify the types of lesions and to allow a systematic approach to treatment options.
Based on a radiological classification, they were initially divided according to the flow dynamics, into low-flow malformations (venous, lymphatic, and capillary lesions), and high-flow malformations (AVM and arteriovenous fistula). Later, the International Society for the Study of Vascular Anomalies (ISSVA), and based on cellular features, flow characteristics, and clinical behaviour, categorized these lesions as simples (capillary, lymphatic, and venous) or combined vascular malformations (AVM, capillary-venous malformation, capillary-lymphatic-venous malformation, lymphatic-venous malformation, capillary-lymphatic-arteriovenous malformation). [2-3]
Therefore, AVMs are a type of vascular malformation. They can occur anywhere in the body but most often occur in the head and neck (40% of the cases). [1-2]
Although most of the AVMs are congenital and occur as a result of aberrant vessel angiogenesis. The confluence of small tortuous vessels is called a nidus, where arteriovenous shunting occurs. [1-3]
Most of them are not be seen at birth and generally increase proportionally in size as the child grows. [2] This growth rate can be exacerbated by hormonal changes or as a result of thrombosis, infection, and trauma. [3]
AVMs can be asymptomatic if small but most of the patients complain of pain, decreased joint mobility, and may have cutaneous changes. [1] Typically on examination, these lesions produce a pulsatile, red, warm mass with a trill [3], but if small they may pass undetected.
Ultrasound can do the initial diagnosis, particularly when the patient presents with a lump. Color Doppler imaging permits analysis of arterial and venous flow and their velocities. Although it is limited in the assessment of deep lesions. [2-6] Therefore MRI represent an important tool for the assessment and classification of these type of lesions.
Such as described in our case, AVMs classically consist of tangles of enlarged arteries and veins, associated with a cluster of malformed high-flow vessels (“nidus”). The Doppler US shows low-resistance arterial waveforms (high velocities) with arterialized venous waveforms. MR imaging classically shows numerous flow voids on spin-echo images and flow-related enhancement on gradient-echo and time-of-flight images, as in our case. Due to shunting, associated draining veins show early enhancement relative to adjacent uninvolved veins. [1-3, 6]
The management of digital AVMs is largely dependent on the severity of symptoms, and if asymptomatic surveillance is often sufficient. The low incidence of AVMs in the digit can present diagnostic and treatment challenges to clinicians. [1]
Written informed patient consent for publication has been obtained.
Arteriovenous malformation
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.







Based on the ultrasound and magnetic resonance imaging (MRI) provided by the patient, a small mass-like lesion is observed in the first toe interspace of the right foot. Doppler ultrasound shows:
MRI sequences show:
In summary, the lesion on ultrasound and MRI demonstrates high-flow vascular mass characteristics, suggesting a high likelihood of an arteriovenous fistula or arteriovenous malformation (AVM).
Taking into account the patient’s age, symptoms (local pain and numbness), physical examination findings (a palpable small mass), and the high-flow arteriovenous shunting seen on ultrasound and MRI, the most likely diagnosis is:
Arteriovenous Malformation (AVM) in the first toe interspace of the right foot.
Depending on the lesion size, symptom severity, and vascular flow characteristics, subsequent management may include interventional treatments (e.g., embolization) or surgical excision. Close follow-up may be considered if the lesion is small and symptoms are mild.
If symptoms are mild and imaging evaluation confirms no extensive involvement of bone or tendon structures, moderate rehabilitation exercises can be implemented. The following is recommended based on the FITT-VP principle:
If the patient experiences significant pain, local redness, or increased numbness, exercise should be temporarily discontinued, and a follow-up evaluation should be conducted. For patients with osteoporosis or a history of foot surgery, a gradual approach is recommended to prevent stress-related injuries.
This report is a reference analysis based on the currently provided information and should not replace an in-person consultation or professional medical judgment. Specific treatment plans should be determined by specialized clinicians in conjunction with the patient’s individual condition.
Arteriovenous malformation