Lipoma arborescens of the knee joint: Typical imaging features



Clinical History
A 51-year-old male presented with a three-year history of left knee pain and sensation of knee instability. Physical examination revealed joint effusion and pain in the medial and lateral compartments of the left knee. There was no history of trauma.
Imaging Findings
A plain radiograph of the left knee revealed degenerative changes in the medial femorotibial and patellofemoral compartments, evidenced by joint space narrowing, marginal osteophyte formation, and a subchondral cyst in the patella. Furthermore, in the lateral view, there was an opacification in the suprapatellar pouch of the knee (Figures 1a and 1b).
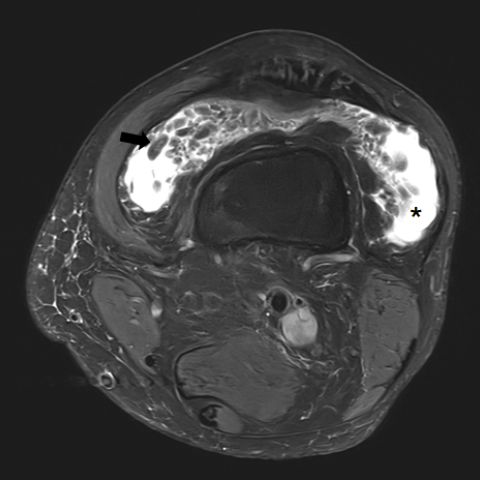
Magnetic resonance imaging (MRI) showed a large-volume joint effusion, with frond-like diffuse synovial thickening, most prominently in the suprapatellar pouch (Figures 2a, 2b and 2c). The thickened synovium demonstrated a signal pattern consistent with fat, exhibiting high signal intensity on T1-weighted sequences and low signal intensity on fat-saturated sequences (Figures 2a, 2b, 2c and 3). Additionally, medial and lateral meniscus tears were identified (Figures 4a, 4b and 4c).
Discussion
Background
Lipoma arborescens (LA) is a rare benign disorder characterised by the proliferation of mature adipocytes within the synovial membrane [1]. This condition usually affects a single joint, most commonly the knee joint, specifically the suprapatellar pouch [2]. However, it has also been documented in other joints, such as the shoulder, hip, elbow, and wrist [3].
The aetiology of LA is not completely understood, but current theories suggest a reactive fatty proliferation of the synovium in response to degenerative or inflammatory arthritis [4,5].
Clinical Perspective
LA is most commonly diagnosed in the fifth to seventh decades of life, although it can occur in younger people with arthritis [6]. Patients usually present with insidious and painless swelling of the affected joint, with intermittent joint effusion [1,7]. Due to its nonspecific clinical presentation, imaging is crucial for accurate diagnosis [8].
Imaging Perspective
Plain radiograph is usually the first image modality to evaluate musculoskeletal pathology. However, in the case of LA, the findings are unspecific. Osteoarthritic changes, which include joint space narrowing, osteophytes, subchondral sclerosis, and subchondral bone cyst formation, are the most common associated imaging findings. Regarding the knee joint, a soft-tissue opacity in the suprapatellar pouch is frequently seen [3].
MRI is the imaging modality of choice for diagnosing LA due to its superior contrast resolution and ability to characterise fatty tissues [5,8]. MRI shows frond-like synovial projections with fat signal intensity on all sequences, namely high signal intensity on T1 and T2-weighted images, which suppress on fat-saturation sequences [2,5]. Following gadolinium administration, peripheral enhancement is observed, corresponding to the thickened synovium, while the subsynovial fatty tissue shows no enhancement. Frequently associated imaging findings include joint effusion and degenerative joint changes, as well as meniscal tears in the knee [5].
There are no magnetic susceptibility artefacts from haemosiderin deposition, which is a typical feature of tenosynovial giant cell tumours [7]. The presence of multiple intra-articular cartilaginous loose bodies, exhibiting varying degrees of calcification and ossification, is more suggestive of synovial chondromatosis [2]. Rheumatoid arthritis shows diffuse synovial thickening and enhancement but lacks the characteristic fat signal intensity of LA [9].
Outcome
The primary goals of the treatment are symptomatic relief and prevention of joint damage. Intra-articular injection of corticosteroids can be used to manage a symptomatic LA. However, synovectomy is the gold standard treatment, allowing the removal of the lipomatous tissue and the improvement of joint function [1]. Follow-up is typically advised to monitor for potential recurrence, which is rare [5].
Take Home Message
- Lipoma arborescens (LA) is characterised by the proliferation of mature adipocytes within the synovial membrane, most commonly affecting the knee joint.
- MRI is the preferred imaging modality for accurate diagnosis, showing characteristic frond-like synovial projections with fat signal intensity.
- Synovectomy is the treatment of choice, with patients typically experiencing low recurrence rates.
Written informed patient consent for publication has been obtained.
Differential Diagnosis List
Final Diagnosis
Lipoma arborescens
Liscense
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Figures
Radiograph


Fat-suppressed proton DWI


MRI T1-weighted

MRI: Associated findings



Medical Imaging Analysis Report
1. Radiological Findings
The patient is a 51-year-old male with persistent left knee pain and a feeling of joint instability for 3 years, without a clear history of trauma. Based on the provided X-ray and MRI images, the following observations are noted:
- Significant intra-articular soft tissue mass exhibiting lobulated or flocculent proliferation, showing high signal on both T1- and T2-weighted MRI sequences. The signal is notably suppressed in fat-suppression sequences, indicating that the lesion is primarily composed of fatty tissue.
- Prominent fat-like proliferation within the knee joint cavity (particularly in the suprapatellar pouch), with the proliferations appearing frond-like or lobulated at the margins.
- There is moderate joint effusion, and degenerative changes are observed in the articular cartilage. These include mild narrowing of the joint space, subchondral sclerosis, and the formation of small osteophytes.
- No clear signs of bony destruction or fracture are observed.
2. Potential Diagnoses
Based on the radiological appearance and clinical history, the following differential diagnoses are considered:
- Lipoma Arborescens
Characteristics: A benign mesenchymal lesion marked by intra-articular fatty proliferation, commonly found in the knee joint. MRI shows a fatty signal, often accompanied by joint effusion and degenerative changes. - Synovial Chondromatosis
Characteristics: Typically seen as multiple cartilaginous or calcified bodies within the joint. MRI reveals cartilaginous signals with small focal calcifications or ossifications, often described as “rice-like” and multiple in number. - Pigmented Villonodular Synovitis (PVNS) / Tenosynovial Giant Cell Tumor
Characteristics: The synovium commonly shows villous hyperplasia. T2-weighted images may exhibit heterogeneous signal intensity, with hemosiderin deposition leading to magnetic susceptibility artifacts (blooming). The imaging typically shows a “mixed” signal. - Rheumatoid Arthritis
Characteristics: Diffuse synovial thickening with enhancement, but no fatty signal. It is often associated with significant inflammatory response. Clinically, it commonly affects multiple joints and may present with systemic symptoms.
3. Final Diagnosis
Taking into account the patient’s age, symptoms, and imaging findings (particularly the presence of frond-like or lobulated fatty signal that is suppressible on fat suppression sequences), and after excluding other conditions such as synovial chondromatosis, PVNS/tenosynovial giant cell tumor, and rheumatoid arthritis, the most likely diagnosis is “Lipoma Arborescens.”
4. Treatment Plan and Rehabilitation
Treatment Strategies:
- Conservative Treatment: For patients with mild symptoms, intra-articular corticosteroid injection may be considered to reduce inflammation and pain.
- Surgical Intervention: The typical approach involves arthroscopic or open synovectomy to completely remove the proliferative fatty synovium, thus preventing further joint damage. In cases of significant clinical symptoms or functional limitation, this should be actively considered.
- Follow-up Observation: After surgery, regular follow-up is recommended to monitor for recurrence or changes in joint function. The recurrence rate for Lipoma Arborescens is relatively low, but long-term follow-up is still necessary.
Rehabilitation/Exercise Prescription Recommendations:
During both pre- and post-operative periods or during conservative management, individualized and progressively adjusted exercises are essential to maintain or restore joint range of motion and muscle strength. Below is a suggested phased plan for reference:
- Early Recovery Phase (after pain relief):
- Frequency: 3–4 times per week
- Intensity: Low intensity, avoiding excessive weight-bearing
- Duration: 20–30 minutes per session
- Methods: Straight leg raises, isometric knee exercises (in sitting or supine positions with slight knee flexion, performed within a safe range)
- Mid-Stage Functional Strengthening (after basic recovery of joint mobility):
- Frequency: 3–5 times per week
- Intensity: Moderate intensity; gradually increase resistance using bands or light weights
- Duration: 30–40 minutes per session
- Methods: Knee flexion and extension exercises, half squats in seated or supine positions, open- and closed-chain lower limb exercises, ensuring proper knee alignment
- Late Consolidation Phase (after improving joint stability):
- Frequency: 3–5 times per week
- Intensity: Moderate-to-high intensity, avoiding high-impact activities
- Duration: 40–60 minutes per session
- Methods: Appropriate walking or cycling, level or gentle uphill training, strengthening quadriceps and hamstring endurance
Throughout these phases, if the patient has risks such as osteoporosis, compromised cardiopulmonary function, or post-operative complications, adjustments to exercise intensity and mode should be made under the guidance of professional rehabilitation therapists and physicians to ensure safety.
Disclaimer: This report is based solely on the currently available clinical and imaging information and does not replace in-person consultation or professional medical advice. The specific treatment plan should be determined by a specialist, taking the patient’s actual condition into consideration.
Human Doctor Final Diagnosis
Lipoma arborescens